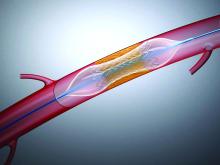
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.