A more recent study tested a collaborative care model, integrating sleep specialists with PCPs to enhance patients’ sleep disorders management. Patients with sleep complaints in the intervention group underwent a one-time consultation with a sleep specialist who provided diagnostic feedback and treatment recommendations to the patient and his/her PCP, in contrast to the control group consisting of usual primary care (UPC). Results showed that provider-initiated sleep-focused interventions were significantly higher in the intervention group for PSG, and mental health clinic referrals. Intervention recipients also showed increases in sleep efficiency and improved ESS scores at the 10-month follow-up. This demonstrates that a one-time sleep consultation, with access to, and oversight from, a specialist sleep center can serve to increase health-care providers’ attention to sleep problems. Subsequently, it increases sleep disorders screening and diagnosis and results in benefits to patients’ sleep/wake symptoms (Edinger et al. Sleep. 2016;39[1]:237).
Integration of sleep centers and primary care
As noted above, the quality of sleep medicine-related care that patients are receiving under our current model is suboptimal. In order to better fit the requirements of the ACA and provide integrated and coordinated sleep medicine care for our patients, we must consider refining our model of sleep medicine delivery by taking the steps below:
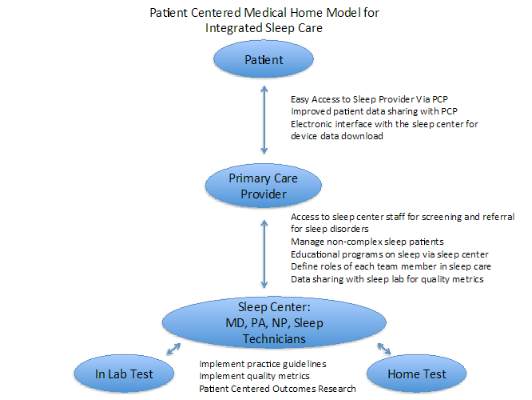
• Encourage partnership of sleep centers with primary care services to develop an integrated care paradigm for sleep medicine by placing PCPs at the center of our sleep care delivery model.
• Educate PCPs on the importance of sleep health, and provide them with appropriate access to resources for sleep testing.
• Allow PCPs to refer patients to a comprehensive sleep program that will be integrated in a PCMH model, providing HST, which will discourage referrals to independent home testing companies that do not offer comprehensive care.
• Strengthen and expand our sleep medicine teams within sleep centers and primary care centers by integrating trained nurse practitioners and physician assistants, who can serve as a resource for PCPs, and reduce fragmentation of care, thereby reducing costs of unnecessary testing.
Conclusions
In summary, the ACA has and will continue to impact sleep care delivery in the United States. An integrated sleep care model will result in not only meaningful improvements in the quality of sleep disorders care, but it will also help diagnose a vastly underdiagnosed condition. It will do so via a PCP-based model, providing access to sleep providers and sleep testing, yet it will encourage and educate the PCP to screen and treat noncomplex sleep disorders in their own practices. Below, we provide an example of this model. Patients via this model will have appropriate access to comprehensive sleep care that will reduce fragmentation of care. This PCMH sleep model is necessary in this post-ACA era that demands primary care provider-based, coordinated, high quality care.
Dr. Kundel and Dr. Shah are with the Division of Pulmonary, Critical Care, and Sleep Medicine, Icahn School of Medicine at Mount Sinai, New York, NY; and Dr. Shah is with the Department of Epidemiology and Population Health, Albert Einstein College of Medicine, Bronx, NY.