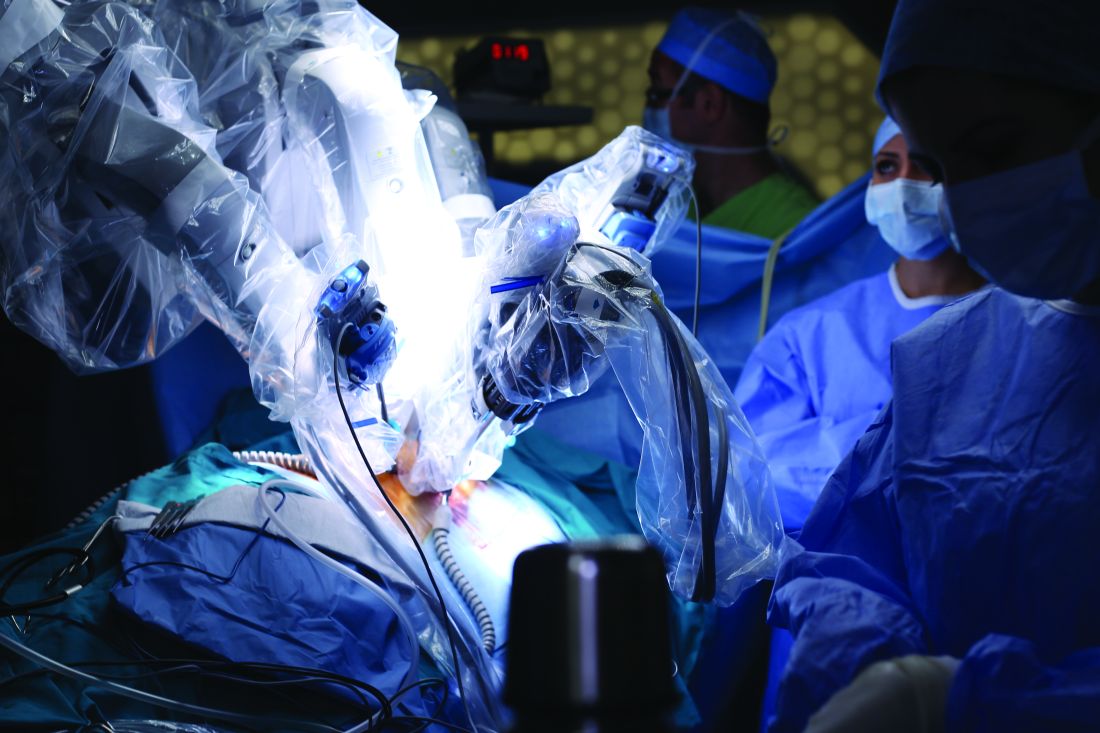
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
The 1- and 3-year survival rates for patients with tumors less than 5 cm were 91% and 84%; they were 86% and 75% in patients with tumors from 5 to 7 cm, and 76% and 47% in patients with tumors larger than 7 cm, respectively. A tumor size larger than 7 cm was significantly associated with both worse 1-year and 3-year survival, compared with patients with a tumor less than 5 cm (P = .004).Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.