Case
A 29-year-old man presented to the ED with a 3-day history of constant left-sided low back pain that radiated to his left buttock and groin. The patient stated the pain worsened with movement, making it difficult for him to walk. He reported lifting heavy boxes at work, but denied any trauma. The patient also denied recent fevers, chills, chest pain, dyspnea, abdominal pain, urinary or fecal incontinence, weakness, numbness, or saddle anesthesia. Regarding his medical history, he had an appendectomy as a child, but reported no other surgeries or medical issues. His social history was significant for narcotic and inhalant use and daily tobacco use. The patient also reported taking heroin intravenously (IV) 6 months prior.
Vital signs at presentation were: heart rate (HR), 92 beats/min; respiratory rate, 15 breaths/min; blood pressure, 118/80 mm Hg; and temperature, 98.2°F. Oxygen saturation was 98% on room air.
The patient was a well-developed young man in no apparent distress. Dermatological examination showed bilateral track marks in the antecubital fossa. The musculoskeletal (MSK) examination demonstrated left gluteal tenderness to palpation and decreased active and passive range of motion of the left hip, especially with internal rotation and flexion. He had no midline tenderness, and the lower extremities had normal pulses and no motor or sensory deficits.
The patient’s pain improved with IV fluids, diazepam, and ketorolac, and he was able to ambulate with assistance. He was clinically diagnosed with sciatica, and discharged home with prescriptions for diazepam and ibuprofen. He was also instructed to follow-up with an orthopedist within 7 days from discharge.
The patient returned to the ED the following day with similar complaints of unabating left-sided pain and difficulty ambulating. His vital signs were notable for an elevated HR of 106 beats/min. Physical examination findings were unchanged from his presentation the previous day, and an X-ray of the lumbar spine showed no abnormalities.
After receiving IV analgesics, the patient’s pain improved and his tachycardia resolved. He was discharged home with instructions to continue taking diazepam, and was also given prescriptions for prednisone and oxycodone/acetaminophen. He was instructed to follow-up with an orthopedist within 24 hours.
Over the next 9 days, the patient was seen twice by an orthopedist, who ordered imaging of the lumbar spine, including a repeat X-ray and contrast-enhanced magnetic resonance imaging (MRI), both of which were unremarkable. The patient completed the prescribed course of diclofenac, oxycodone/acetaminophen, and prednisone, but experienced only minimal pain relief. The orthopedist prescribed the diclofenac to supplement the medication regimen that he was already on.
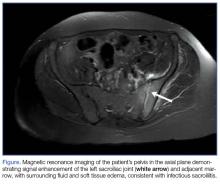
At the second follow-up visit, the orthopedist ordered an MRI of the patient’s left hip, which demonstrated inflammation of the left sacroiliac joint (SIJ) with effusion, and a 1-cm by 1-cm collection adjacent to the left psoas muscle; these findings were concerning for septic arthritis (Figure). Based on the MRI study, a computed tomography (CT)-guided arthrocentesis of the left SIJ was performed by an interventional radiologist.
Following the arthrocentesis, the orthopedist referred the patient to the ED. At this presentation, the emergency physician (EP) ordered blood cultures, blood work, urinalysis, and a urinary toxicology screen, and started the patient on IV ceftriaxone and vancomycin. The laboratory studies were significant for the following elevated inflammatory markers: erythrocyte sedimentation rate (ESR), 19 mm/h; C-reactive protein (CRP), 2.45 mg/L; white blood cell count (WBC), 13.6 K/uL with normal differential; and lactate level, 2.6 mg/dL. The toxicology screen was positive for opioids. The basic metabolic panel, chest X-ray, and urinalysis were all unremarkable. An electrocardiogram showed sinus tachycardia.
The patient was admitted to the hospital, and infectious disease services was contacted. While awaiting transport to the inpatient floor, the patient admitted to IV drug use 4 weeks prior to his initial presentation—not the 6 months he initially reported at the first ED visit.
The blood cultures grew Candida parapsilosis, and culture from the SIJ arthrocentesis grew Pseudomonas aeruginosa. The infectious disease physician switched the patient’s antibiotic therapy to IV cefepime and fluconazole. The patient also was seen by an orthopedist, who determined that no surgical intervention was required.
Follow-up laboratory studies showed inflammatory markers peaking at the following levels: ESR, 36 mm/h; CRP, 4.84 mg/L; and WBC, 32.1 K/uL with 90% neutrophils. These markers normalized throughout his hospital stay. The patient was also tested for hepatitis and human immunodeficiency virus, both of which were negative. A transesophageal echocardiogram showed no obvious masses or vegetations.
The patient had an uncomplicated hospital course, and was discharged home on hospital day 6 with a 4-week prescription of oral fluconazole and levofloxacin, and instructed to follow-up with both infectious disease and the orthopedist. To address his history of IV drug use, he also was given follow-up with pain management.
One month later, the patient returned a fourth time to the ED for evaluation of bilateral lower extremity pain and swelling. He stated that he had been mostly bed-bound at home since his discharge from the hospital due to continued pain with weight-bearing.
The patient’s vital signs were normal. The EP ordered a duplex ultrasound study, which showed extensive bilateral lower extremity deep vein thrombosis. He was started on subcutaneous therapeutic enoxaparin and admitted to the inpatient hospital. During admission, a left lower lobe pulmonary artery embolism was found on chest CT angiography, though he had no cardiac or respiratory symptoms. He was discharged home with a 3-month prescription for oral rivaroxaban.
At a 4-month follow-up visit, the patient reported minimal residual disability after completing the course of treatment. During the follow-up, the patient denied using IV heroin; he was referred to a pain management specialist, who placed the patient on methadone.
Discussion
Infectious sacroiliitis (ISI) is a rare form of infectious arthritis affecting the SIJ, with an incidence of 1 to 2 reported cases per year.1 The literature on ISI currently consists only of case reports and case series. This infection is often diagnosed after the disease has progressed, with a mean time to diagnosis of 43.3 days.2
Infectious arthritis of any joint has a prevalence of 2 to 10 per 100,000 people. In 50% of cases, the knee is the joint most commonly affected, followed by the hip, shoulder, and elbow.3 Regardless of location, infectious arthritis is associated with significant morbidity and mortality due to sepsis and irreversible loss of joint function.4
Risk factors for ISI include IV drug use, pregnancy, trauma, endocarditis, and immunosuppression.1 The decision to initiate the workup for ISI can be difficult to make because the condition may present without signs of an infectious etiology, such as toxic appearance, inflammatory changes surrounding the joint, or even fever—only 41% of affected patients in one case series were febrile.2 The workup is often time-consuming, invasive, and expensive.
Although delayed diagnosis and treatment of septic arthritis is associated with significant adverse effects, there is unfortunately no consensus to guide the workup for ISI. As opposed to Kocher’s criteria for the differentiation of septic hip arthritis from transient synovitis in pediatric patients or well-known red-flags for further evaluation of low back pain, physicians are left without much guidance when considering laboratory workup or imaging decisions to evaluate for ISI.
Sacroiliac Joint
As previously noted, the SIJ is not commonly affected by infection. It is a diarthrodial, L-shaped joint comprised of the posterior ilium and sacrum, and is a near-rigid structure with very limited movement that provides stability to the axial skeleton.5 The SIJ is often overlooked as a secondary cause of low back pain in younger patients with rheumatologic conditions (eg, ankylosing spondylitis, Reiter syndrome), pregnancy-associated ligamentous laxity, and osteoarthritis in elderly patients. In one study, 88.2% of sacroiliitis cases were inflammatory, 8.8% infectious, and 2.9% degenerative.6
Signs and Symptoms
As our case illustrates, ISI often presents with nonspecific symptoms and physical findings.7 Patients typically present with fever, painful manipulation of the SIJ, and unilateral lumbo-gluteal pain.2 The components of the history and physical examination suspicious for an infectious etiology include the subacute presentation; unresolved pain despite treatment; tenderness to palpation; decreased range of motion; and recent IV drug use, which increases the risk of infectious disease due to unsterile practices and direct inoculation of pathogens into the bloodstream8 and a further predilection into the axial skeleton. 9 It is important to obtain an accurate social history; however, patients may not be forthright about disclosing sensitive information such as sexual history and illicit drug use.
Physical Assessment
The SIJ is best appreciated in the seated patient by palpating one fingerbreadth medial to the posterior superior iliac spine as he or she slowly bends forward.10 Tenderness elicited while in this position is suggestive of SIJ inflammation. The area of tenderness may be lower than anticipated and lateral to the gluteal cleft, as synovial fluid is typically relegated to the lower half of the joint.
Several adjunctive physical examination maneuvers, such as the Gaenslen test and Flexion Abduction External Rotation test (FABER test or Patrick’s test) can isolate SIJ pathology or dysfunction. The Gaenslen test is performed by asking the patient to lie supine and flex the affected hip and knee, with the lumbar spine flat against the examination table. Hyperextending the contralateral thigh downward will reproduce pain in the affected SIJ.
The FABER test is a simple but less specific examination technique to assess joint pain in the hip, lumbar, and sacroiliac joints.11 In this assessment, the clinician flexes the patient’s affected knee to 90°, externally rotates the hip, and applies downward pressure on the knee. Pain reproduced in the affected SI region is sensitive for joint inflammation.
Laboratory and Imaging Studies
Laboratory studies typically show inconsistent and nonspecific findings, such as the elevated ESR and CRP levels seen in our patient.2,12 Imaging studies to assess the SIJ for signs of infection are therefore essential for confirming infection.
Magnetic resonance imaging is the preferred imaging modality to assess for ISI, since it has the highest sensitivity in visualizing joint effusion and bone marrow edema compared to other modalities. Computed tomography, however, can be helpful in visualizing associated abscesses and guiding arthrocentesis.12 Plain X-ray may not demonstrate early changes in bone.13 The confirmatory study for ISI is synovial fluid analysis and culture.7
Treatment
Infectious sacroiliitis secondary to P aeruginosa, a gram-negative bacillus, is difficult to treat because of the glycocalyx and slime production that protects the pathogen from antibiotics, the development of multiple-antimicrobial resistance, and poor drug penetration into bones and abscesses.14 Antibiotic treatment should cover Staphylococcus aureus and may be broadened to cover gram-negative bacilli. The recommended duration of treatment is at least a 2-week course of IV antibiotics, followed by a 6-week course of oral antibiotics.2 Therapy also includes pain control and surgical intervention for abscesses, osteomyelitis, and refractory cases.7
Complications
Complications and long-term sequelae are common in ISI, often due to late diagnosis of the condition. Our case illustrates the delayed diagnosis of Pseudomonas ISI with candidemia in a young man with a history of IV drug use presenting with atraumatic low back pain. His clinical course was complicated by a thromboembolic event, likely secondary to immobility and a hypercoagulable state from infection and inflammation.15 Infectious sacroiliitis secondary to P aeruginosa is most commonly seen in patients with immunosuppression, hospitalization, and IV drug use.2
Summary
Infectious sacroiliitis remains a diagnostic challenge for physicians due to its rare incidence and nonspecific clinical manifestations. Our case illustrates the importance of maintaining a high level of clinical suspicion for infectious arthritis in young patients presenting with common MSK complaints in the presence of infectious risk factors. Emergency physicians should consider red flags, abnormal vital signs, and patient recidivism when deciding on the most appropriate workup.