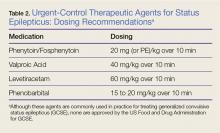
All patients without an identifiable secondary cause of GCSE (eg, hypoglycemia, hyponatremia, hypocalcemia) should be started on a second-line agent. Treatment with a second-line agent provides two benefits: First, patients who experience resolution of seizure activity may rapidly attain therapeutic levels of AEDs, which may be sustained through maintenance therapy; and second, the second-line treatment may abort refractory cases of status.12 Table 2 provides dosing recommendations for second-line agents.
Phenytoin and Fosphenytoin
Phenytoin and the newer prodrug fosphenytoin are a mainstay urgent-control therapy for emergency physicians (EPs) and neurologists alike. In one of the few head-to-head studies of AEDs,13 phenytoin did not perform as well as the other study agents (diazepam, lorazepam, and phenobarbital); however, generalizability from this study is limited. Fosphenytoin continues to be an efficacious choice for second-line treatment of AED.
Fosphenytoin, a water-soluble prodrug of phenytoin, is given preferentially over IV phenytoin due to its decreased risk of cardiovascular (CV) side effects and more rapid administration.14 Moreover, fosphenytoin is compatible with most IV fluids (eg, dextrose, lactated Ringer’s solution, normal saline [NS]), whereas phenytoin is only compatible with NS. For convenience, fosphenytoin is dosed in phenytoin equivalents (PE/kg)—eg, administration of 20 PE/kg over 10 minutes is a potential loading dose for fosphenytoin.
Valproic Acid
Valproic acid has become a favored second-line agent for many providers due to its relatively safe profile and rapid infusion time. Most studies have shown IV valproic acid is at least as effective as phenytoin, but data continue to be somewhat weak and most of the studies are uncontrolled.15
Hepatotoxicity is generally only associated with long-term use of valproic acid, but it remains reasonable to abstain from using this agent in patients with preexisting hepatic disease. Valproic acid toxicity can lead to somnolence, ataxia, seizures, and coma with marked hyperammonemia.16
Levetiracetam
Intravenous levetiracetam is becoming a more commonly used drug both for emergent initial treatment of seizure and as a maintenance therapy. While data on levetiracetam are limited, a few studies tout the efficacy and safety of IV loading to abort GCSE.
In observational studies, levetiracetam appears to have similar efficacy to other AEDs and may be more beneficial in early therapy.17 An ongoing current study, The Emergency Treatment With Levetiracetam or Phenytoin in Status Epilepticus trial, is examining a prospective cohort of pediatric patients comparing levetiracetam against phenytoin.18
Levetiracetam is generally considered safe. The most commonly reported side effects are dizziness, somnolence, nausea, and brief transaminitis.19 Levetiracetam has also been associated with neuropsychiatric exacerbations.20
Phenobarbital
Intravenous phenobarbital has been used as an urgent-control therapy for seizure with good efficacy, even in recent years.21 Despite this, phenobarbital may cause profound CV depression necessitating the use of vasopressors.22 Large-dose phenobarbital can be used to induce coma in patients, although this should not be attempted without the guidance of a neurologist. While phenobarbital can be used safely in certain circumstances, its use has fallen out of favor in the ED due to the availability of safer alternative options.