Diabetes mellitus (DM) affects about 347 million people worldwide, making it the new global epidemic. 1 In the U.S alone, the number of adults with DM has more than tripled over the past 30 years. Now, almost 10% of the U.S. population has the disease and is at risk for serious systemic complications, including blindness. 2
Diabetes is the leading cause of new cases of legal blindness in adults aged 18 to 74 years in the U.S. Diabetic retinopathy, seen as vascular changes in the retina related to DM, is found in almost half of all patients with DM. 3 As the number of people with DM is expected to increase, so is the number of people affected with and blinded by diabetic retinopathy. Providers in both primary care and subspecialty settings have a critical role to play in the management and prevention of blindness in diabetic patients.
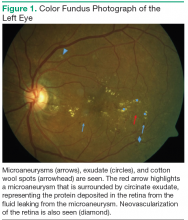
According to the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR), diabetic retinopathy will affect 99% of patients with type 1 DM (T1DM) and 60% of patients with type 2 DM (T2DM) after 20 years of having diabetes. 4 Diabetic retinopathy is a result of the microvascular damage that occurs from diabetes. The most common findings seen on a dilated fundus exam in nonproliferative diabetic retinopathy are microaneurysms, intraretinal hemorrhages, hard exudates, and cotton wool spots (Figure 1). Cotton wool spots represent focal areas of retinal ischemia. Nonproliferative disease progresses to proliferative retinopathy when neovascularization develops.
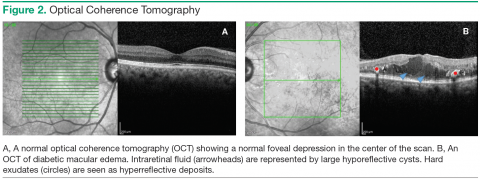
One of the major causes of vision loss in the setting of DM is diabetic macular edema (DME). Between 4% and 7% of people with DM currently have DME. 5,6 Diabetic macular edema is a result of the break down of the bloodretinal barrier, which is an extension of the blood-brain barrier. Hyperglycemia causes a disruption of the cellular tight junctions, pericyte loss, and thickening of the basement membrane. These changes cause weakness in the walls of the retinal blood vessels, allowing microaneurysms to form. Hyperglycemia also causes upregulation of the production of inflammatory markers such as vascular endothelial growth factor (VEGF), protein kinase C, prostaglandins, and cytokines, which increase retinal vascular permeability (Figure 2). 7
Risk Factors for DME
Several studies have found the prevalence of DME to be higher in black (10.4%-15.6%) and Hispanic (18%) patients vs non-Hispanic white patients (6.3%-8.4%); Asian patients have the lowest prevalence of DME (5%). 5,6,8,9 The modifiable risk factors for the development of DME include hyperglycemia, duration of disease, hypertension, and dyslipidemia. Patients who have had DM for a longer period of time (> 10 years) and those with a higher hemoglobin A 1c (A 1c ) are more likely to have DME. 4,6 The WESDR showed that for each percentage point increase in baseline A 1c, there was a 28% increase in the incidence of visual impairment at the 25-year follow-up. 10 An A 1c < 7% is recommended in patients, though some may benefit from an A 1c < 6.5%. 11
Epidemiologic studies have also found hypertension and dyslipidemia to be associated with an increased risk of DME. 12-15 Both diseases lead to an increased vascular permeability, compounding the microvascular damage already present from DM. In hypertension, DME and retinal hemorrhages are thought to be influenced by the increased perfusion pressure in retinal vessels. 16 For every 10 mm Hg increase in blood pressure over 160 mm Hg, the risk of DME increases by 25%. 17 Dyslipidemia contributes to DME by damaging endothelial cells and causing increased vascular permeability through cytokine and VEGF upregulation. 18