The VHA is the largest single provider of human immunodeficiency virus (HIV) care in the U.S., with over 26,000 HIV-positive veterans in care in 2013. 1 HIV care in the VHA is delivered across 152 hospitals and nearly 1,400 health care facilities, including
community-based outpatient clinics, skilled nursing facilities, veteran centers, rehabilitation centers, hospices, and domiciliaries in the U.S. and its territories. 2
The structure of HIV care in the VHA has been described in more detail elsewhere and, for context, is briefly highlighted here. 3 Many veterans with HIV infection receive both HIV care and primary care through an infectious disease or HIV specialist, whereas others receive HIV care and primary care in separate clinics. Every medical center has a designated HIV lead clinician who serves as the point of contact for the VHA National HIV Program. This network facilitates rapid dissemination of policy changes and clinical updates to HIV providers nationally, as well communication to the National HIV Program about barriers and challenges to providing high-quality care at the local level. The National HIV Program monitors and evaluates comprehensive HIV care programming, which includes increasing HIV testing, availability of pre-exposure prophylaxis, and access to and quality of comorbidity care (for more information on VHA HIV care, please visit: http://www.hiv.va.gov).
Comorbidity care is a particular focus of the National HIV Program. The majority of veterans with HIV in VHA care are now in late middle-age; in 2011, 66% were aged between 50 and 69 years. 4 As the population of veterans with HIV grows older, age-related chronic medical comorbidities (eg, diabetes mellitus, cardiovascular disease) and mental health considerations (eg, cognitive impairment, depression, substance use) become increasingly critical areas of clinical focus at the individual and the population level.
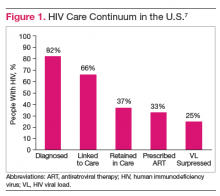
The HIV care continuum provides a useful model to conceptualize critical components of providing high-quality comprehensive HIV clinical care, including diagnosis, linkage to care, retention in care, prescription of antiretroviral therapy (ART), and viral suppression. Achieving virologic suppression is the primary goal of HIV care. It decreases morbidity and mortality for the HIV-infected individual and decreases the risk of transmission to others. 5
This continuum of care is used increasingly by federal agencies and other health care systems to assess engagement at each critical juncture. The Centers for Disease Control and Prevention has estimated that, due to significant drop-offs between each step of the continuum, only 25% of the 1.1 million people living with HIV in the U. S. are virally suppressed (Figure 1). 6,7
Recently, the HIV care continuum cascade was used to assess HIV care within a VA medical facility. 8 The authors assessed performance along the HIV care continuum at the Atlanta VAMC (AVAMC) Infectious Disease Clinic, an urban clinic providing care to over 1,400 veterans with HIV. Using an independent stage categorization analysis, they found that the AVAMC outperformed national estimates at every stage of the HIV care continuum. Notably, 62.8% of the clinical population diagnosed with HIV was prescribed ART and 52.3% had achieved viral suppression, more than double the national rate (Figure 2). 8-10