The VACHS clinic model incorporated: (1) regular clinic visits and follow-up with laboratories and imaging for 5 years, based on National Comprehensive Cancer Network (NCCN) guidelines; (2) monitoring for psychosocial distress at each visit, using a modified version of the NCCN Distress Thermometer, and a registered nurse or health tech documenting scores in CPRS with a templated Distress Screening note; (3) referrals to nutrition, health psychology, social work, physical therapy, smoking cessation, and the palliative care team as appropriate; (4) education about diagnosis, risk factors, and healthy living; and (5) reviewing the SCP to each patient.
The VACHS approach was designed to be patientcentered by incorporating individualized surveillance and screening guidelines, wellness education tailored to cancer type and treatment history, psychosocial support for survivors and their families through individual therapy and support groups for patients and families, and individual exercise and fitness recommendations through physical therapy and pulmonary rehabilitation referrals.
Needs Assessment
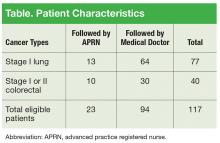
The VACHS cancer care coordinator worked with the tumor registrar to generate an initial referral patient list. Patients were identified in the tumor registry who met these criteria: diagnosed with stage I lung cancer or stage I or II colorectal cancer and treated at VACHS between 2008 and 2012. Initial research showed that there were 117 patients followed in the VACHS hematology/oncology clinic in the fall of 2012 who met the criteria. At that time, 80% of the patients identified were being followed by an attending oncology physician and 20% by an oncology APRN (Table).
Based on this initial analysis, the projected patient load for this clinic was anticipated to be 100 patients annually with between 2 and 4 annual visits each. Of note, in 2013 VACHS started a low-dose chest computed tomography screening program for patients who met high-risk criteria. The number of patients diagnosed and treated for stage I non-small cell lung cancer at VACHS during 2014 and 2015 was more than double the number treated in 2012.
Partnering With IT
The VACHS cancer care coordinator contacted the VISN 1 clinical application coordinator (CAC) in October 2012 who then reached out to her counterpart in Boston, where the sample CPRS template from the survivorship toolkit (toolkit template) was being tested. In November 2012, the VACHS CAC loaded the toolkit template into the test folder of the template drawer of VACHS CPRS. Changes were made over time to shorten the toolkit template to include the relevant information using the shortest number of words.
The template was modified by deleting 3 sections. The appointment list and the medication list were eliminated from the template as it was felt that these change with each visit. The psychosocial distress assessment also was eliminated as this score was known to change from visit to visit.
A separate initiative was undertaken simultaneously to address the need to monitor oncology patients for psychosocial distress regularly. Health psychology providers at VACHS used the NCCN Distress Thermometer to monitor distress in oncology patients. The team elected to take the distress assessment language out of the SCP and create a separate note template to record the distress scores for VACHS patients. The group chose the note titles Cancer Survivor Treatment Summary and Patient Distress Screening to clarify the purpose of the notes and to make searching CPRS or VistA for the note titles easier for providers or researchers.