Dr. Fehnel, this patient’s initial cerebrospinal fluid (CSF) cell count and chemistries were completely normal. Is this sufficient to rule out encephalitis? If not, what other diagnostic tests would you send?
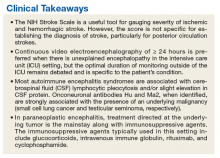
►Dr. Fehnel. A fully normal CSF profile reduces the likelihood of a broad range of neuro-infectious etiologies but does not completely rule those out. For example, there are reports of herpes simplex virus (HSV) encephalitis producing relatively normal profiles and even negative polymerase chain reaction assays for antibodies to HSV if the specimen is obtained very early in the course of the disease.3,4 That was not the case here as the CSF was obtained several days after his initial presentation. Given this patient’s clinical syndrome, normal CSF findings, and long smoking history without regular screening examinations, I would send a CSF specimen screening for paraneoplastic and autoimmune encephalitis. Most autoimmune encephalitis syndromes are associated with CSF lymphocytic pleocytosis or slight elevation in CSF protein levels. This patient’s diagnosis is most likely an anti-Hu paraneoplastic syndrome, which can be distinguished from other autoimmune and paraneoplastic processes by the characteristically normal CSF profile. Anti-Hu antibodies are strongly associated with non-small cell lung cancer (NSCLC). I would, therefore, also obtain more advanced chest imaging.
►Dr. Li. An autoimmune and paraneoplastic encephalitis panel was sent. While this send-out panel was pending, a CT torso was obtained to evaluate for occult malignancy in light of his significant smoking history. This showed a 3-cm spiculated mass originating from the left hilum. Bronchoalviolar lavage washings returned positive for small cell lung cancer.
The CSF autoimmune encephalitis panel returned positive for anti-Hu antibody. A final diagnosis of paraneoplastic encephalitis secondary to small cell lung cancer was made.Dr. Fehnel, can you explain the mechanism by which certain neoplasms can cause encephalitis?
►Dr. Fehnel. Onconeuronal antibodies Hu (NSCLC) and Ma2 (testicular seminoma), when identified, are strongly associated with the presence of an underlying malignancy. The work of Dr. Josep Dalmau and others in this area has dramatically improved our understanding of these syndromes over the past 25 years.5 The exact mechanism is not fully understood but is thought to be mediated by cytotoxic T-cell response directed at the malignancy itself with homology to intraneuronal structures, which are readily absorbed and result in neuronal cell death.6
►Dr. Li. Is there a specific treatment for paraneoplastic encephalitis, other than treating the underlying malignancy?
►Dr. Fehnel. Early treatment is associated with improved outcome and should not be delayed while waiting for laboratory confirmation in cases of high clinical suspicion. Treatment directed at the underlying tumor is the mainstay along with less specific immunosuppressive agents. Unfortunately Anti-Hu (as well as Ma2) antibodies are intraneuronal and less responsive to standard treatments relative to other paraneoplastic auto-antibodies identified on the cell surface. Immunosuppressive agents typically used in this setting include high-dose IV methylprednisolone, IV immune globulin (IVIG), rituximab, and cyclophosphamide.7
►Dr. Li. The patient was started on IVIG, methylprednisolone, cisplatin, and etoposide. His course was complicated by aspiration pneumonia, autonomic dysfunction causing tachy- and brady-arrhythmias, urosepsis, worsening somnolence, chemotherapy-induced neutropenic fevers, and ultimately septic shock. The palliative care team was closely involved throughout the final stages of his hospital course. After multiple family meetings, the patient was transitioned to comfort-focused care per family discussion and died 6 weeks after his initial presentation.