Selecting level of care and ICU management
Patients with predicted severe AP or those with persistent SIRS despite initial fluid resuscitation should be managed in a closely monitored unit, ideally an ICU. Patients with impending respiratory failure require mechanical ventilation, renal failure complicated by metabolic acidosis and/or hyperkalemia requires hemodialysis, and cardiovascular shock requires the initiation of vasopressors and continuous monitoring of blood pressure via an arterial line. A special entity that requires ICU level care is hypertriglyceridemia (HTG)-induced severe AP. HTG should be considered as the etiology of AP in certain clinical scenarios28: previous history of HTG, poorly controlled diabetes mellitus, history of significant alcohol use, third trimester of pregnancy, and use of certain medications associated with HTG such as oral estrogens, tamoxifen, and propofol. Levels of triglyceride greater than 1000 mg/dL strongly point toward HTG being the etiology.
Plasmapheresis, which filters and removes triglycerides from plasma, has been reported as an efficient treatment in such patients based on case series29,30. At this time its use may only be justified in patients with predicted severe AP from HTG, preferably within the first 24 hours of presentation.
Urgent ERCP
Urgent ERCP (within 24-48 hours of admission) in patients with biliary AP is indicated31 when there is strong clinical suspicion for concomitant cholangitis and/or evidence of ongoing biliary obstruction (secondary to choledocholithiasis) on imaging. Currently, predicted severe AP of biliary etiology does not constitute an indication of urgent ERCP in the absence of the above parameters32.
Nutrition
Recovery of the gut function is often delayed for several days or weeks in patients with severe AP. Studies have shown that prolonged fasting in such circumstances leads to malnutrition and worse prognosis33,34. Enteral nutrition via a nasogastric (NG) or nasojejunal (NJ) tube is the preferred route of nutritional support, as it is associated with lower risk of infection, multi-organ failure, and mortality when compared to total parenteral nutrition33.
The question of whether NJ feeding offers any additional advantages over NG feeding has not been clearly answered with a recent randomized trial showing NG feeds not to be inferior to NJ feeds35. In regards to the timing of initiation of enteral nutrition, early nasoenteric feeding within 24 hours from presentation was found not to be superior compared to on-demand feeding in patients with predicted severe AP36.
Strategies to decrease risk of recurrent attacks
The etiology of AP can be determined in the majority of patients. In many instances, recurrence can be prevented, i.e., in biliary or alcoholic etiologies. In patients with mild biliary AP, evidence supports37 the performance of cholecystectomy during the index admission. In cases of severe biliary AP complicated by pancreatic necrosis and/or peripancreatic fluid collections, cholecystectomy should be delayed for a few weeks until the collections regress or mature38. In poor surgical candidates, ERCP with biliary sphincterotomy offers an alternative, but less effective, means of reducing the risk of recurrent attacks in patients with biliary AP39. In subjects with first AP attack of alcoholic etiology, counseling focusing on alcohol cessation has shown to reduce risk of recurrences40. Similarly, appropriate plans to treat and follow-up underlying metabolic etiologies (hypercalcemia and HTG) should be preferably instituted prior to the patients’ discharge.
Management of peripancreatic fluid collections
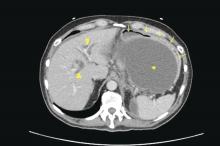
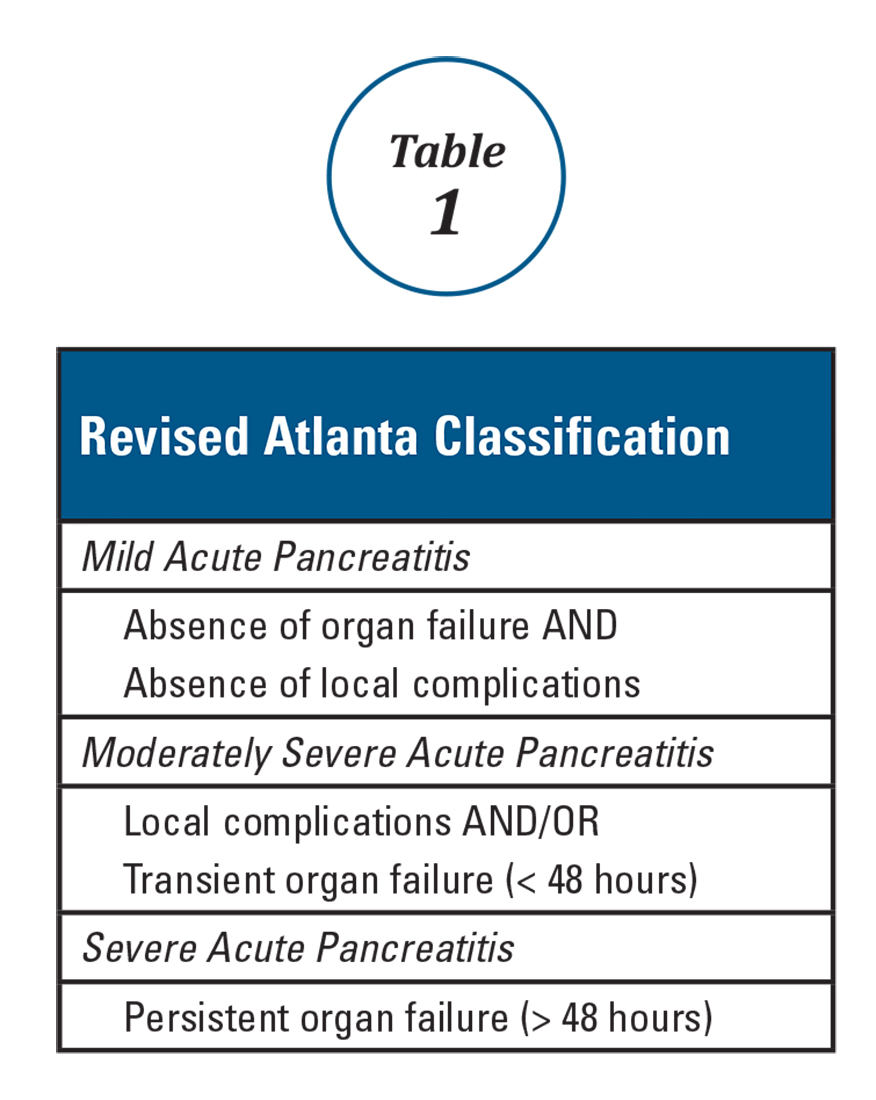
Patients with AP frequently develop peripancreatic fluid collections (PFCs). Based on the revised Atlanta classification, those are categorized into four types (Table 2, Figures 1-4).
The majority of acute PFCs in patients without evidence of pancreatic necrosis regress within a few weeks and thus intervention is not indicated early in the disease course. Current literature supports delaying the drainage/debridement of such collections for several weeks. The mortality from interventions decreases as the time to intervention from onset of symptoms increases41. Delaying intervention gives more time for recovery from systemic complications and allows the encapsulating wall and contents to organize further.
It is only the mature PFCs, which are symptomatic resulting in abdominal pain, nausea, early satiety, gastric outlet obstruction, failure to thrive, and/or biliary obstruction, that need to be drained/debrided42. Minimally invasive approaches have shown to result in better outcomes when compared to open laparotomy. Minimally invasive approaches include placement of percutaneous drainage catheters by interventional radiology (retroperitoneal approach preferred when feasible), endoscopic drainage/debridement, laparoscopy, and retroperitoneal necrosectomy following a step-up approach43.
While surgery is still an option for patients with symptomatic mature PFCs, endoscopic ultrasound-guided drainage in expert hands has been shown to be cost effective, with shorter hospital stay and even decreased risk of cyst recurrence compared with surgical cyst-gastrostomy creation44. Ultrasound or computed tomography-guided drainage of such collections with a percutaneous catheter is an equally efficacious option when compared to the endoscopic approach. However, patients undergoing endotherapy require fewer procedures and imaging studies and shorter length of stay45 when compared with radiological interventions.