Welcome to the new Practice Management Toolbox.
The AGA Practice Management and Economics Committee (PMEC) is pleased to host an updated Practice Management Toolbox column featuring contemporary GI practice management issues and news. As chair of the PMEC, I am excited to bring you this content on behalf of my colleagues on the committee. Each month we will highlight a timely topic relevant to gastroenterologists in practice. The AGA and PMEC strive to be at the forefront of changes to the field of gastroenterology, providing you with tools and resources to succeed. If there is an article topic you would like to suggest, please reach out to Jacob Manthey, Practice and Quality Manager at jmanthey@gastro.org .
Anton Decker, MD, AGAF
Chair, Practice Management and Economics Committee
Last year, Medicare began laying groundwork for major changes to coding and payment for common evaluation and management (E/M) services and two high-volume GI endoscopy procedures beginning January 1, 2021 with expected adoption by commercial payers. Learn about these potential changes now to help prepare your practice for the financial impact.
2021 E/M Changes: New guidelines, new payments
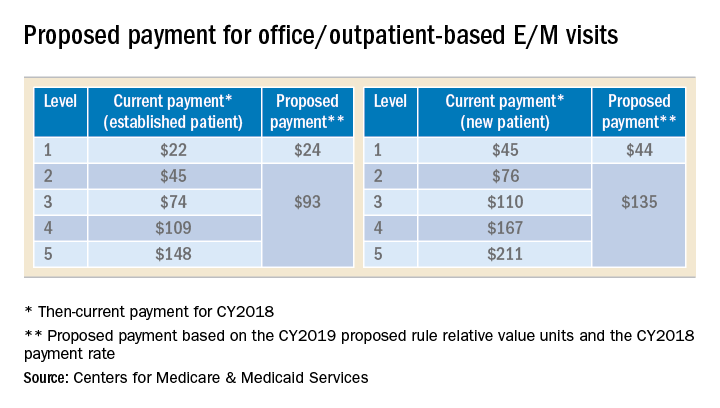
The Centers for Medicare and Medicaid Services (CMS), also commonly referred to as Medicare, announced in its 2019 Physician Fee Schedule proposed rule that it wanted to reduce administrative burden and improve payment accuracy for office/outpatient new and established patient codes (99201-99205 and 99211-99215) by paying level 2–5 codes at a single payment rate and simplifying documentation to support only a level 2 E/M visit, except when using time for documentation (Table).
In the original proposal, those who reported mostly level 2 and 3 E/M visits would have experienced modest payment increases while those who reported mostly level 4 and 5 E/M visits would have endured payment cuts between 20%-40%. Ultimately, the physician community, including AGA and its sister societies, opposed the proposed payment consolidation and pressured CMS not to finalize most of its proposed changes and preserve the current payment rates. The 2019 MPFS final rule made no changes to the relative values for office/outpatient new and established patient codes 99201-99205 and 99211-99215, but did outline a new plan “for paying a single rate for E/M office/outpatient visit levels 2 through 4 for established and new patients while maintaining the payment rate for E/M office/outpatient visit level 5 in order to better account for the care and needs of complex patients.” CMS agreed to continue to accept input on improvements to the proposal before CMS’ planned implementation in 2021.
A proposal to simplify E/M guidelines within Current Procedural Terminology (CPT) and preserve the individual levels of the new and established patient office/outpatient E/M codes, except 99201 which was proposed for deletion, was presented to the American Medical Association (AMA) CPT Editorial Panel, the body responsible for creating and maintaining CPT codes, and approved at its February 2019 meeting. The approved changes will not be publicly available until the CPT 2021 book is released in August 2020. In the meantime, the AMA Specialty Society Relative-value scale Update Committee (RUC) will make recommendations to CMS on potential new relative values for the E/M codes.
It is unclear whether CMS will accept the AMA CPT Editorial Panel’s changes and potential new values or move forward with the plan for three levels of E/M for office/outpatient new and established patient codes. However, any changes to the current guidelines will undoubtedly involve a learning curve for both physicians and coders and it is unclear whether approximately four months from the time the 2021 CPT book is released and the time the new rates will be implemented on January 1, 2021 is enough to master the changes and update internal systems. In addition, any changes to reimbursement will impact each practice’s bottom line.