Patient navigation as a best practice for GI procedures
Colonoscopy is the preferred method for colorectal cancer (CRC) screening. Among scheduled outpatient colonoscopies, key metrics like no-show rates and poor bowel preparation can be as high as 25% in some facilities. These missed appointments and repeated calls with patients have been an important source of wasted resources, poor patient outcomes, and revenue loss for endoscopy facilities (estimated to be up to $1 million dollars for 10-member GI practice).
Studies have shown that patient navigation (PN), a patient-centered approach, overcomes barriers in health care delivery, thus improving adherence to CRC screening. Typically, navigators are specialized health practitioners who fill a variety of functions, including providing updates and instructions to patients, as well as assisting with test-related fears. Despite the overall cost-effectiveness, PN programs require significant resources from hospitals or medical groups. The continued focus in the United States on value-based medicine has provided an urgent need for cost-effective treatments that are also readily available to most physicians.
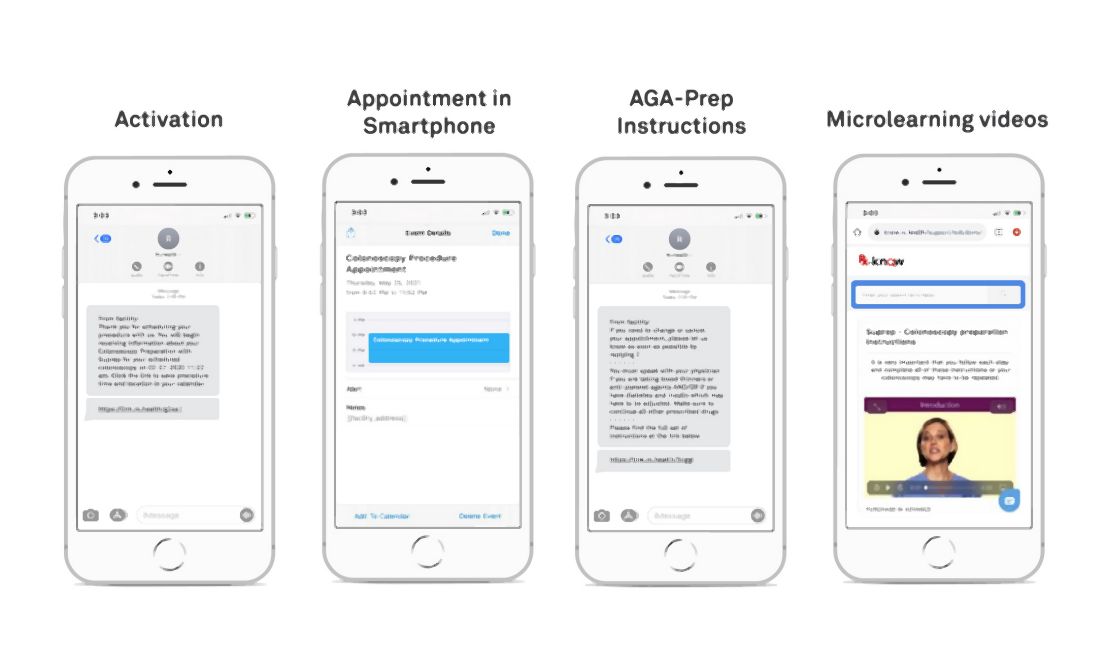
Digital navigation to automate navigation for colonoscopy and other GI procedures
(see Figure below). Given the widespread use of mobile phones, DN has the ability to change the way doctors and health care providers work. This led to Mount Sinai Health System, New York, conducting a quality improvement program to automate and evaluate the effectiveness of an automated text messaging and web-based “digital navigation” platform for decreasing colonoscopy appointment no-show rates.
If a valid phone number was available in the patient’s electronic medical record chart and they did not opt out of receiving text message communications from the Mount Sinai Health System, patients over the age of 18 years who were scheduled for a colonoscopy at either of Mount Sinai Hospital, Mount Sinai Morningside, or Mount Sinai West were automatically sent DN SMS messages. The RxUniverse software platform (Rx.Health, New York) was used to send DN content through SMS to all eligible patients. The software platform interfaces with the EMR and endoscopy system (Provation) to automatically extract patient phone number and appointment details.
Impact of digital navigation and patient engagement
This study at Mount Sinai Health System demonstrated that patient engagement with SMS-based navigation is strongly predictive of colonoscopy completion. Patients with high engagement with digital navigation are about four times more likely to complete colonoscopy. Of all covariates included in the model, high DN engagement level had the largest effect size (odds ratio, 3.97), compared with no engagement. For health systems with patient navigators, targeting patients who are unlikely to engage DN or are low-engagers may be a more efficient use of person-to-person navigation.
Value-based reimbursement and cost-effectiveness have emerged as core principles in American health care reform, possibly requiring the creation of affordable, cost-effective approaches. Our research at Mount Sinai Health System suggested that SMS-based navigation can be a potential cost-effective strategy for reducing no-show rates. Beyond appointment no-shows, adequate bowel preparation is another important component of the preprocedure navigation process. Insufficient bowel preparation requires a repeat procedure, as poor visualization of the colon results in reduced therapeutic benefit from screening colonoscopy. We’ve shown in previous studies that our DN platform can increase bowel preparation efficiency, which results in lower rates of aborted procedures.
Missed colonoscopies not only cause longer wait times for patients, but they also cost the average facility $725 a day in lost revenue. It has been found through studies that traditional PN is cost-effective, with additional revenue generated from increased colonoscopy completion rates exceeding the costs of program implementation. While formal cost analyses have not been conducted on DN, estimates have shown around $1 million in annual savings for an average ambulatory surgery center or 10-member GI practice.