SAN DIEGO – Laparoscopic sleeve gastrectomy is positioned between gastric banding and the laparoscopic gastric bypass for both safety and efficacy, results from the largest comparative study of its kind demonstrated.
The finding comes at a time when the Centers for Medicare and Medicaid Services is reviewing evidence to consider including sleeve gastrectomy as a covered benefit. Currently, gastric bypass, vertical banded gastroplasty, duodenal switch, and gastric banding are the only CMS-sanctioned bariatric procedures.
The study, which involved nearly 300,000 patients, "shows that across the board, regardless of the procedure, bariatric surgery is safe and effective," Dr. John M. Morton said in an interview at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "The emerging new procedure, the sleeve gastrectomy, is shown to be right between the bypass and the band. As a result, we have seen more interest from payers to cover it. In fact there are about 100 million lives that are covered. Our only outlier is CMS in deciding to cover. We hope that these data will help influence CMS in granting coverage for the sleeve gastrectomy."
Dr. Morton, associate professor of surgery and director of bariatric surgery at Stanford Hospitals and Clinics at Stanford (Calif.) University, and his associates examined BOLD (Bariatric Outcomes Longitudinal Database) to identify patients who had undergone laparoscopic Roux-en-Y gastric bypass (LRNYGB), gastric banding (LAGB), and sleeve gastrectomy (LSG) from June 2007 to December 2010. BOLD, the largest bariatric-specific database, is maintained by the ASMBS Bariatric Surgery Center of Excellence program, and includes more than 1,200 surgeons at 540 hospitals. Dr. Morton described the data as a "clinically rich" variable set that includes age, gender, race, insurance status, body mass index, excess body weight, and comorbidities.
"There is a definite need for more data around comparison of different procedures," Dr. Morton said at the meeting. "Our study hypothesis is very straightforward: Do demographics and outcomes for bariatric surgery vary by procedure?"
The primary outcomes were 30-day mortality, serious complications, and readmissions. The definitions of serious complications included death, anastomotic leakage, cardiac arrest, deep venous thrombosis, evisceration, heart failure and/or pulmonary edema, liver failure, and bleeding requiring transfusion.
Dr. Morton reported outcomes from 117,365 patients in the LAGB group, 138,222 in the LRNYGB group, and 16,139 in the LSG group. Patients in each group were generally the same age (a mean of 45, 46, and 45 years, respectively), mostly female (78%, 79%, and 74%), and mostly white (72%, 73%, and 72%). "The one area where there was a sizable difference was around self-pay," Dr. Morton said. About 21% of patients in the LSG group paid out-of-pocket, compared with 6% of those in the LAGB group and 2% of those in the LRNYGB group.
The proportion of preoperative comorbidities was similar among the three groups, with two exceptions. The prevalence of diabetes was highest in the LRNYGB group (37%, compared with 30% in the LSG group and 28% in the LAGB group; P less than .0001). A similar association was seen in the proportion of patients with five or more preoperative comorbidities (62%, 55%, and 52%, respectively; P less than .0001).
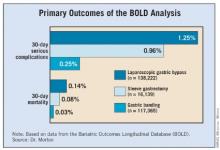
The mean length of stay was 0.7 days for the LAGB group, 1.9 days for the LSG group, and 2.3 days for the LRNYGB group. The percent change in BMI at 12 months was 7.6%, 13.4%, and 16.4%, respectively; the rate of 30-day serious complications was 0.25%, 0.96%, and 1.25%; and the rate of 30-day mortality was 0.03%, 0.08%, and 0.14%. All differences between the groups were significant (P less than .0001).
"If you look at the remainder of the safety outcomes – everything from 30-day readmission to 30-day reoperation – it’s pretty much the same order, with the band group having the lowest [percentage], and the bypass having the highest, and the sleeve being right in between," Dr. Morton said. "When we looked at age greater than 65 in isolation, we found that the order of safety remains, with the banding having the least amount of mortality and the sleeve being right between the band procedure and the bypass."
Logistic regression analysis revealed several significant factors that predicted serious adverse events at 30 days: male gender (odds ratio, 1.67), having nonprivate insurance (OR, 1.15), stepwise progression with increasing age (for example, an OR of 1.27 for those aged 26-35 years and an OR of 4.42 for those above age 65), and stepwise progression with increasing BMI (for example, an OR of 1.37 for those with a BMI of 46-55 kg/m2 and an OR of 3.03 for those with a BMI greater than 65).