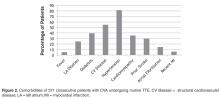
In addition to reviewing echocardiogram reports, all patient records were evaluated for clinical variables including age, gender, presence of atrial fibrillation, hypertension, diabetes, past CVA, left atrial dilation by calculation of indexed direct left atrial volume, recent myocardial infarction, and known cardiovascular disease.
All echocardiograms were performed on Hewlet-Packard Vivid 7 or Vivid 9 (GE Healthcare, Wauwatosa, WI) by technicians who held registered diagnostic cardiac sonographer status. All TTEs contained the “standard” views in accordance with published guidelines [10].Saline contrast to look for shunts was not standard on these studies. Echocardiogram images were stored digitally and read from an EchoPac (GE Healthcare, Wauwatosa, WI) reading station. All echocardiograms were interpreted by one of 16 American Board of Internal Medicine–certified cardiologists, 5 of whom were testamurs (physicians who have passed one of the examinations of special competence in echocardiography). These 5 interpreted 20% of the studies.
Results
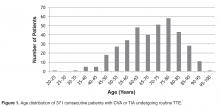
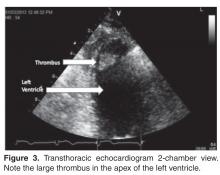
During the observation period, 867 patients with a diagnosis of CVA or TIA were admitted to our institution. Among these patients, there were 417 TTEs performed as part of their evaluation, generally within 48 hours of the event or admission. Over 90% of the TTEs were ordered by hospitalists, who were responsible for admitting patients to the stroke unit at our institution. Forty-six of the patients were subsequently felt not to have had a CVA or TIA on clinical grounds by their treating physicians in conjunction with absence of brain imaging findings, and were excluded from further analysis. Hence, the remaining cohort was comprised of 371 consecutive TTE studies for CVA or TIA that was documented on clinical and imaging criteria The population contained 49.9% men and 50.1% women. The average age was 69.7 years (range, 23–96). The age distribution is further outlined in Figure 1 . The remainder of the demographic and clinical variables are outlined in Figure 2 . The mean CHADS-VASC score [11] was 4.2. Of the 371 echocardiograms, only 1 showed an unequivocal source of embolism, specifically a left ventricular apical thrombus in a patient who had recently experienced an anterior myocardial infarction ( Figure 3 ).
Discussion
Our data are in keeping with those of others, though our yield was even lower than that reported in previous studies [1–3]. The low yield may be explained by a number of factors. First, we did not include patent foramen ovale or atrial septal aneurysms (which account for a high percentage of embolic sources in other publications) since there is not a clear consensus that any of those entities are associated with an increased risk of embolic events. The exclusion of cardiomyopathy as a cause of CVA or TIA is arguable, but its link to CVA or TIA is also unproven. One study did associate cardiomyopathy with CVA [12]; however, the mechanism is not clear, as the incidence of CVA in cardiomyopathy has been described as similar regardless of the severity of left ventricular dysfunction [13].Many past reports have come from tertiary care centers, where there may be referral bias whereas our data come from consecutive patients at a single community hospital.