The mean number of barriers from the barriers checklist was 9.2 (SD = 10.1) out of 53 possible. Sixty-five participants (86%) reported at least 1 barrier to accessing health care (Table 2). The most frequently cited barriers to care were provider knowledge and attitudes, followed by transportation, insurance, and access to services (eg, hours and location of services). Less frequently cited barriers to care were individual barriers, including memory, health literacy and motivation, as well as those related to SCD itself, ie, fatigue and pain.
Sociodemographic Variables, Emotional Distress, and Health-Related Quality of Life
Symptoms of anxiety and depression were highly correlated with one another, as would be expected ( r = 0.75, P < 0.001). Physical and mental HRQL were significantly correlated with symptoms of depression ( r = –0.67, P < 0.001 for physical HRQL component and r = –0.70 for mental HRQL component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of depression. Physical and Mental Component Summary scores were significantly correlated with symptoms of anxiety ( r = –0.58, P < 0.001 for the physical component and r = –0.62 for the mental component, P < 0.001), with impaired HRQL in both domains correlated with greater symptoms of anxiety. Ratings of difficulty with daily functioning from depressive symptoms were correlated with impaired HRQL in the physical ( r = –0.46, P < 0.01) and mental domains ( r = –0.52, P < 0.001). Ratings of difficulty with daily functioning from anxiety symptoms were also correlated with impaired HRQL in the physical ( r = –0.58, P < 0.001) and mental domains ( r = –0.63, P < 0.001). Reports of more barriers to health care were significantly correlated with reports of more depressive and anxiety symptoms ( r = 0.53, P < 0.001 and r = 0.48, P < 0.001), with lower Mental Component Summary scores ( r = –0.43, P < 0.05), and with more ED visits in the past year ( r = 0.43, P < 0.05).
Relations Between Independent Variables and Outcomes
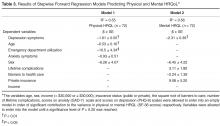
Results of regression analyses ( Table 3 ) indicated that a model including depression symptoms, age, ED utilization, anxiety symptoms and sex predicted the physical component of HRQL (R 2 = 0.55, F(5, 66) = 15.8, P < 0.001). Increased symptoms of depression, older age and 3 or more ED visits in the previous 12 months were independently associated with lower ratings of physical HRQL, controlling for anxiety and sex. A model including depression symptoms, barriers to care, insurance status, lifetime complications of SCD and sex predicted the mental component of HRQL (R2 = 0.56, F(5, 66) = 16.7, P < 0.001). Increased symptoms of depression were independently associated with lower ratings of mental HRQL, controlling for barriers to care, insurance status, lifetime complications of SCD, and sex.Discussion
Results of this study showed that as expected, symptoms of depression were independently associated with the mental component of HRQL, controlling for other variables. Symptoms of depression were also independently associated with the physical component of HRQL. The effect size for both models was moderate but comparable to effect sizes of other studies of predictive models of physical and mental HRQL in SCD [49]. Our findings were consistent with previous literature, with older age and increased ED utilization independently associated with lower ratings of physical HRQL, with sex and anxiety symptoms entering into the predictive model [15–18,44,45]. Contrary to our hypotheses, barriers to accessing health care were not independently associated with physical or mental HRQL but did contribute to the model for mental HRQL, as did clinical complications and private insurance status.