Discussion
Evidence of patient characteristics that consistently predict suboptimal glycemic control during hospitalization is needed to better inform clinical decisions for inpatient glycemic management. Hospitalized patients would greatly benefit from glycemic protocols that incorporate risk stratification tools based evidence-based risk factors for poor glycemic control [12]. The science of inpatient glycemic management is in its infancy, however, and currently there is limited evidence to help identify at-risk populations and guide effective management for at-risk patient populations [13]. This study provides important data that can be used to develop risk stratification tools with implications for improved glycemic management of hospitalized patients with diabetes. Among the 32 factors included in the final multivariate logistic model (Table 2), 10 were statistically significant predictors of SGC. The top 3 predictors of SGC were HbA1c, admission blood glucose, and steroid use. These are straightforward, easily accessed factors that can become the basis for effective risk stratification and targeted clinical therapies.
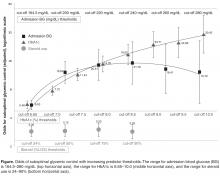
This study showed that the degree of diabetes control prior to admission, as measured by HbA1c, is one of the strongest predictors of inpatient SGC. Patients with poorly controlled diabetes pre-admission had significantly higher rates of SGC than patients admitted with good diabetes control. Furthermore, there was a strong linear relationship between degree of pre-admission diabetes control and glycemic control during hospitalization: the higher the HbA1c on admission, the higher the odds are for poor glycemic control during hospitalization (Figure). The odds of SGC increased more than fivefold at an HbA1c of just 6.7% (50 mmol/mol) and continued to increase linearly as HbA1c increased. This increase occurred despite the fact that patients with poorly controlled pre-admission diabetes were found to have a significantly greater rate of insulin treatment using standardized order sets (which included basal and rapid-acting insulin) than the total sample in this study. So although patients with poorly controlled diabetes pre-admission were actively managed using evidence-based insulin order sets to control glycemia throughout their hospitalization, this did not translate to better glycemic control. Boord et al [14] and Neubauer et al [15] found similar results in their evaluation of glycemic control in hospitalized patients: while insulin use was high, glycemic control remained suboptimal. Similarly, Schnipper et al [16] found that adherence to insulin orders per se were not associated with better glucose control. They noted that the majority of patients with continued elevated blood glucose values did not have changes made to their insulin orders in response to suboptimal blood glucose values. These observations and this study’s findings suggest that fixed standardized subcutaneous orders may be more effective for well-controlled patients with diabetes than for patients with poorly controlled diabetes on admission. These patients need more frequent modifications to standard order sets based on clinical response during hospitalization to ensure good glycemic control.