Results
Patient Characteristics
Practice samples had slightly more women than men (55.2%), were largely white (95.0%) and 50 years of age on average (mean = 49.53, SD = 20.18). The prevalence of diabetes (10.2%) and cardiac disease (10.4%) was relatively low. The percentage of women (56.3%) and whites (96.4%) for the patient level analytic samples was similar to the practice samples, whereas the prevalence of diabetes (33.6% ) and cardiac disease (44.6%) was notable higher and patients were more than 10 years older on average (mean = 61.62, SD = 23.96).
Practice Level Outcomes
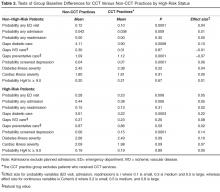
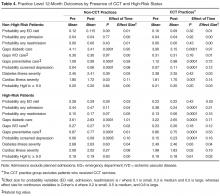
CCT practices were performing significantly better at baseline than non-CCT practices for both non-high-risk and high-risk patients ( Table 3 ), with a lower probability of an ED visit or an unplanned admission, fewer gaps in diabetic care and greater probability of depression screening. There was one exception: CCT practices had significantly more gaps in preventative care at baseline than non-CCT practices but only for non-high-risk patients.Given these group baseline differences and only one instance where the Time by Group interaction was significant where group baseline differences were absent (see below), simple pre-post analyses were conducted for each group separately ( Table 4 ). The results for non-high-risk patients indicated that, in both CCT and non-CCT practices, there was no improvement in utilization, but there were significant reductions in gaps in diabetic and preventative care and cardiac illness severity and significant increases in depression screening, although effect sizes for the latter 2 outcomes were small to negligible.
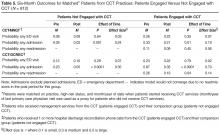
Unlike for non-high-risk patients, there were significant reductions in the probability of an unplanned admission and a 30-day readmission although not an ED visit, but only in CCT practices among high-risk patients. In fact, the one significant Time by Group interaction, F(1,4816) = 32.17, P < 0.001, not affected by group baseline differences pertained to the probability of a 30-day readmission: whereas high-risk patients in CCT practices had a significant reduction in the probability of a readmission, those from non-CCT practices had a marginally significant increase. There were also significant reductions in gaps in diabetic and preventative care, and significant increases in depression screening for high-risk patients in both CCT and non-CCT practices; however, the reduction in cardiac illness severity only held in CCT practices, although, here too, effect sizes for the latter 2 variables were small and negligible.Practice joy fell in the medium range [19] at all time-points, with no notable change over time (see Appendix in the online version of this article). There was also no change in patient satisfaction (see Appendix, online), although after 12 months the “always” response for following up on lab tests was no longer higher than the national comparison and helpfulness of staff rated “never/sometimes” was below the national comparison.