Results
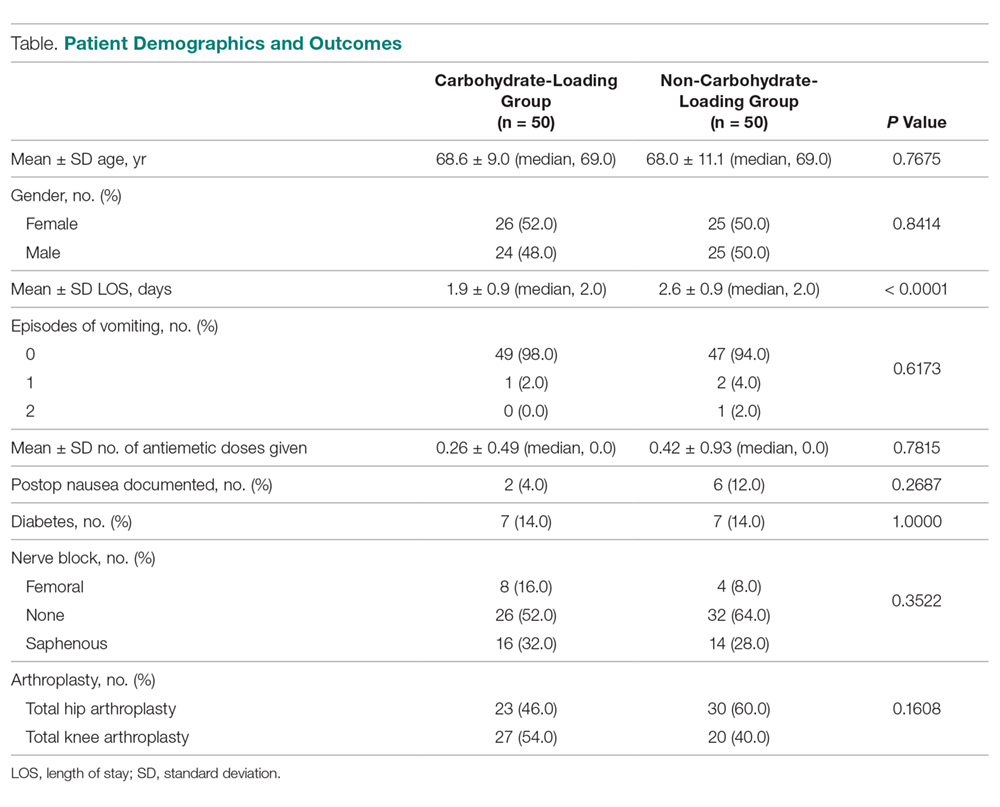
The carbohydrate-loading group (n = 50) and the non-carbohydrate-loading group (n = 50) were comparable for age, gender, type of arthroplasty, episodes of vomiting, diabetes, and nerve block (Table).
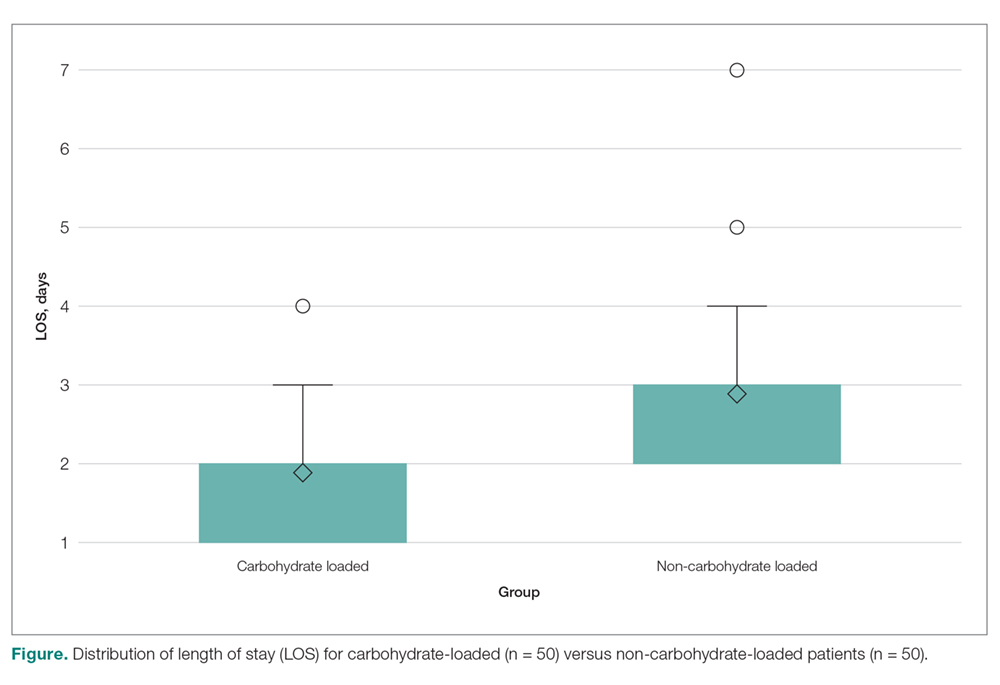
Six different joint replacement surgeons participated in the study. The mean LOS for the carbohydrate-loading group was 1.9 days, while the LOS for the non-carbohydrate group was 2.6 days (difference of 0.7 days; P < 0.0001; Figure). The number of antiemetic medication doses on POD 0 and 1 was evaluated. A total of 13 doses of antiemetic medications were given to the carbohydrate-loaded group and 21 doses were given to the non-carbohydrate group. The average number of antiemetic doses given to a patient postoperatively was 0.26 for the carbohydrate group and 0.42 for the non-carbohydrate group (difference of 0.16 doses; P < 0.7815). There was not a significant difference in the rate of postoperative nausea documented in the carbohydrate-loaded patients as compared to the non-carbohydrate-loaded patients (4% vs 12%, respectively, P < 0.2687).Discussion
In this study we explored whether carbohydrate loading prior to total joint replacement influenced postoperative nausea and LOS in a single institution. The 2 groups appeared similar in terms of demographics as well as the types of surgical procedures performed. After initiation of the carbohydrate-loading protocol, LOS decreased by approximately 1 day. There was also a trend toward decreased usage of antiemetics in the carbohydrate-loaded group, although the final values were not statistically significant. There were also fewer documented cases of postoperative nausea in the carbohydrate-loaded group.
The failure to find a statistical difference in postoperative antiemetic usage between carbohydrate-loaded and non-carbohydrate-loaded patients may be due to incomplete documentation (ie, not all patients who were nauseous having their symptoms documented in the chart). Due to the small number of antiemetic doses given to each patient, we may have lacked the necessary numbers to visualize the difference between the groups. We were unable to perform a post-hoc power calculation with our current data. Additionally, the decrease seen in LOS may not have been due solely to carbohydrate loading, since the data were collected over multiple years during implementation of the ERAS protocol. There is a possibility that the ERAS protocol, which is multimodal, was better implemented as time progressed, adding a confounding variable to our data. Despite these limitations, however, we were able to demonstrate a decreased LOS for patients who underwent total joint replacement with the initiation of a preoperative carbohydrate-loading ERAS protocol. Furthermore, there was a trend toward decreased documented postoperative nausea and decreased antiemetic use in the group that avoided fasting and received carbohydrate supplements.
This decrease in LOS by almost 1 day is consistent with multiple prior studies that demonstrated a similar decrease when implementing an ERAS protocol.3-5,7 The trend towards lower antiemetic use and less postoperative nausea in the carbohydrate-loading ERAS protocol gives merit to further research on this topic, with the goal of finding an optimal preoperative practice that allows patients to experience rapid mobilization, minimal postoperative nausea, and faster recovery overall.
Conclusion
The carbohydrate-loading ERAS protocol implemented at our institution was found to decrease LOS for joint arthroplasty patients by approximately 1 day. Additionally, there was a trend toward decreased antiemetic use and fewer documented cases of postoperative nausea when patients underwent preoperative carbohydrate loading. Further research on carbohydrate loading prior to joint replacement appears warranted, as this may be another avenue to optimize postoperative outcomes in this patient population.
Corresponding author: Christopher L. Blum, MD, Stony Brook Medical Center, Stony Brook, NY; blumc18@gmail.com.
Financial disclosures: None.