Obstructive sleep apnea is a common condition among patients in intensive care units, affecting nearly 8% treated at one large academic medical center during a 3-year period, according to a report published online in the Journal of Critical Care.
In what they described as the first study to document the prevalence of obstructive sleep apnea (OSA) in the ICU patient population, researchers found that 1,183 of 15,077 patients (7.8%) aged 16 years and older who were treated between 2003 and 2006 had a physician-documented diagnosis of OSA at admission. Surprisingly, however, OSA did not raise mortality risk, even though it is a well-known predictor of cardiovascular disease and is strongly associated with several comorbid conditions such as obesity, diabetes, and hypertension, said Dr. Enrique Bolona, a fellow in critical care medicine at the Mayo Clinic, Rochester, Minn., and his associates.
Patients treated in three medical, surgical, and mixed ICUs who had comorbid OSA had significantly lower ICU mortality (2.4%) than did ICU patients without OSA (6.2%), as well as significantly lower hospital mortality (3.9% vs. 11.4%). The OSA group also had a shorter median length of stay (1.13 vs. 1.50 days), the investigators reported (J. Crit. Care 2014 Oct. 10 [doi: 10.1016/j.jcrc.2014.10.001])
Patients with OSA had less severe illness than did ICU patients without OSA, as measured by their lower APACHE III scores (median, 45.3 vs. 54.9), lower scores on the Acute Physiology Scale (median, 35.3 vs. 41.8), and lower predicted mortality at admission (10.3% vs. 16.3%). But even after the data were adjusted to account for this discrepancy between the two patient groups in disease severity, OSA was still associated with significantly lower mortality (odds ratio, 0.40).
The reason for these “unexpected” findings is not yet known. It is possible that obesity, which strongly correlates with OSA, exerts a protective effect during critical illness by virtue of increased nutritional reserves. Data concerning patients’ body mass index were not available, so this hypothesis could not be confirmed, Dr. Bolona and his associates said.
Another possible explanation is that patients with diagnosed OSA have better access to the health care system than nonaffected patients, “resulting in closer follow-up and management of associated comorbidities.
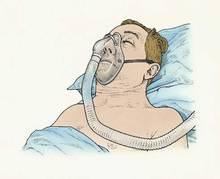
“Once admitted to the ICU, stricter monitoring and a higher level of alertness with regard to detection of respiratory problems may also play a role, making patients with OSA more likely to receive therapies such as noninvasive positive pressure ventilation earlier,” they said.
This study was limited in that it was retrospective and involved only a single medical center. “The generalizability of our results is unknown,” the investigators noted.
Dr. Bolona and his associates reported having no financial disclosures.