Restoring native kinematics of the knee has been a primary goal of anterior cruciate ligament (ACL) procedures. Double-bundle ACL reconstruction, compared to single-bundle, has been hypothesized to more effectively re-establish rotational stability by re-creating the anatomic ACL, but has not yet proven to result in better clinical outcomes.1
In 1879, Dr. Paul Segond described a “fibrous, pearly band” at the lateral aspect of the knee that avulsed off the anterolateral proximal tibia during many ACL injuries.2 The role of the lateral tissues in knee stability and their relationship with ACL pathology has attracted noteworthy attention in recent time. There have been multiple studies presenting an anatomical description of a structure at the anterolateral portion of the knee with definitive femoral, meniscal, and tibial attachments, which helps control internal rotational forces.3-7 Claes and colleagues4 later found that band of tissue to be the anterolateral ligament (ALL) and determined its injury to be pathognomonic with ACL ruptures.
The ALL is a vital static stabilizer of the tibio-femoral joint, especially during internal tibial rotation.8-10 In their report on ALL and ACL reconstruction, Helito and colleagues11 acknowledge the necessity of accurate assessment of the lateral structures through imaging to determine the presence of extra-articular injury. Musculoskeletal diagnostic ultrasound has been established as an appropriate means to identify the ALL.12
Ultrasound can accurately determine the exact anatomic location of the origin and insertion of the ALL. Reconstruction of the ALL could yield better patient outcomes for those who experience concurrent ACL/ALL injury. Here we present an innovative technique for an ultrasound-guided percutaneous method for reconstruction of the ALL and report on a patient who had underwent ALL reconstruction.
Surgical Indications
All patients undergo an ultrasound evaluation preoperatively to determine if the ALL is intact or injured. Our experience has shown that when ultrasound evaluation reveals an intact ALL, the pivot shift has never been a grade III.
Our indications for a combined ACL and ALL reconstruction are a positive ultrasound diagnosis of an ALL tear, and a grade III pivot shift test in an ACL-deficient knee or a grade I-II pivot shift test in an ACL-intact knee (Table 1). The ACL cannot be left insufficient if the patient is to have a successful ALL reconstruction.Surgical Technique
For a demonstration of this technique, see the video that accompanies this article.
The pivot shift test is conducted under anesthesia to determine whether an ALL reconstruction is required. The patient is placed in a supine position with the knee flexed at 30o, at neutral rotation, and without any varus or valgus stress.
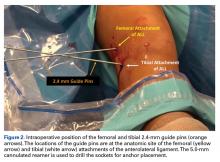
The knee is prepped and draped under sterile conditions. Under ultrasound guidance, the origin and insertion of the ALL are identified and marked with an 18-gauge spinal needle (Figure 1).A No. 15 blade is used to make a small incision centered on each spinal needle. The spinal needle is replaced with a 2.4-mm drill pin (Figure 2).
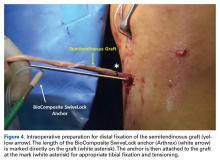
A 90o hemostat is used to establish a plane under the iliotibial (IT) band between the 2 incisions to pass a looped FiberWire suture (Arthrex) for passage of the graft and FiberTape (Arthrex). The FiberTape acts as an internal brace. A socket 22 mm in length is drilled using a 5.0-mm cannulated reamer over each drill pin. A 4.5-mm semitendinosus graft was prepared with a collagen-coated FiberTape attached to a 5.5-mm BioComposite Vented SwiveLock anchor (Arthrex) and fixed into the femoral socket (Figure 3).The graft and FiberTape are then passed under the IT band to the distal incision. Using the length of the BioComposite SwiveLock anchor as a guide, a mark is made on the graft after tensioning the construct in line with the leg, distal to the tibial drill pin (Table 2, Figure 4).
The second 5.5-mm BioComposite SwiveLock anchor is attached to the FiberTape and graft at the mark. The rest of the graft is resected. The BioComposite SwiveLock anchor, graft, and FiberTape are fixed into the tibial socket, completing the reconstruction (Figure 5). Passive range of motion should then be checked to ensure the construct is not overtensioned.Rehabilitation
Rehabilitation following an ALL procedure is similar to traditional ACL rehabilitation with an added emphasis on minimizing rotational torque of the tibia in the early stages.
Our protocol allows for early weight-bearing and minimal use of assistive devices (ie, immobilizer brace and crutches) because an internal brace is performed on every ALL reconstruction. The protocol emphasizes full range of motion and linear power with a progression to lateral and rotational activities. This enables the client to begin rehabilitation within 1 week and regain normal daily function quickly. Return to heavy lifting, physical activity, and sports is delayed until after 6 months to allow for the graft maturity and integration, which takes quite a while, as grafts are weakest after 6 weeks.13 When patients return to sports and activity, a brace is used for up to 1 year postoperatively to limit shearing forces inherent in pivoting and cutting.