Type III Tears: Reconstruction With Remnant Tensioning
The previously discussed techniques have the goals of preserving as much native ligament remnant as possible, approximating the ligament remnant towards the femoral wall, and promoting healing of the ligament. In some cases, however, the ligament remnant is too short for healing (Figure 5A). Although the ligament cannot be approximated to the femoral wall in these cases, there is still an argument for ACL preservation, as was discussed in the first article of this series.
If the ligament length is between 25% and 75% of the native tissue length, the senior author performs a remnant tensioning technique.
The main goal of tensioning the remnant here is to prevent fluid egress into the tibial tunnel and avoid cyclops lesions, while theoretically improving graft vascularization and proprioception. With this technique, 1 or 2 passes are made through the most proximal part of the remnant and the sutures are then parked in an accessory portal as described above. The technique is very similar to that of an augmented repair; however, the graft dimensions here tend to be significantly larger due to the diminished contribution of the remnant. No strength can be expected of this small remnant since it will not be approximated close to the wall. The tibial tunnel is then drilled in standard fashion through the center of the tibial remnant (Figure 5B). After passing the repair sutures through the TightRope RT button of the soft tissue graft, the sutures of the graft and remnant are passed through the center of the distal remnant (Figure 5C). After the passage of the soft tissue graft sutures and button through the femoral socket, the button is flipped, and the graft is delivered. The knee is then cycled and the graft is fixated distally using a BioComposite interference screw. Finally, the remnant is then tensioned as a partial sleeve around the graft (Figure 5D) and tied over the TightRope RT button using alternating half hitches tied with a knot pusher from laterally.Type IV Tears: Reconstruction With Remnant Preservation
Finally, in some cases, the distal remnant is small or the tissue quality in the largest part of the remnant is poor, and after debriding back to good tissue quality, only 10% to 25% of the native tissue length is left (Figure 6A). In these cases, the remnant is preserved, however, tensioning of the remnant with sutures is usually not necessary for the prevention of cyclops lesions. Nonetheless, it is important to debride the parts of the remnant ligament with poor tissue quality as mop-end patterns of the remnant may increase the chance of these lesions (Figure 6B).
In this situation, any of the standard ACL reconstruction techniques can be performed with simple attention being paid to preserving what is left of the tibial insertion site. At the very least, the small insertion remnant guides the anatomic placement of the graft, and prevents egress of joint fluid into the tibial tunnel and could minimize tunnel widening.
Theoretical benefits also include improved vascularity and proprioception. The tunnels are prepared, the grafts passed, and fixation placed per the surgeon’s preference (Figure 6C). The remnant is then arthroscopically checked to confirm that there is no impingement or risk of cyclops lesions (Figure 6D).Type V Tears: Primary Repair
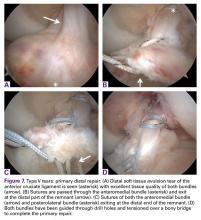
Finally, in some patients a soft tissue avulsion (Figure 7A) or bony avulsion of the distal attachment of the ACL can be seen. Both injuries are relatively rare, although bony avulsions are frequently seen in children, especially those younger than 12 years old. In these cases, the same techniques and theory that are applied to proximal avulsion type tears can be used and applied to distal avulsion type tears.
However, they must be applied in an upside down manner by working from proximal to distal in this case.First, No. 2 FiberWire sutures are passed from proximal towards the distal end of the ligament in the anteromedial bundle, and the same process is then repeated for No. 2 TigerWire sutures for the posterolateral bundle. Then both sutures are exited at the distal avulsed end at the locations of the anteromedial and posterolateral footprints (Figure 7B). A 2.4-mm ACL guide wire and a Ninitol wire are used to drill 2 tunnels from the tibia towards the tibial footprint. The repair sutures are then retrieved through both tunnels (Figure 7C) and the sutures are tied distally over a ligament button after cycling of the knee (Figure 7D). This technique is very useful for soft tissue avulsions, or when there are only small flecks of bone or when the avulsed bone is significantly comminuted. If a large bony avulsion fragment is present, this technique can also be applied with some modification, although there have been multiple other techniques described in the literature that work well in this situation including fixation with screw and washer, or with suture anchors.