Take-Home Points
- MASH is a multicenter arthroscopic study of the hip that features a large prospective database of 10 separate institutions in the United States.
- The mean patient demographic was age 34.6 years, BMI 25.9 kg/m2, 62.8% females, and 97% white.
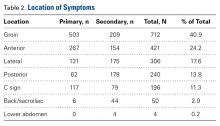
- Most patients had anterior or groin pain, but 17.6% had lateral hip pain, 13.8% had posterior hip pain, and 2.9% had low back or sacral pain.
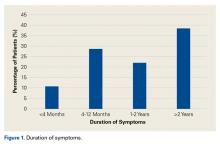
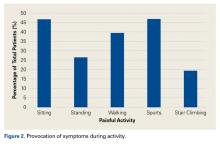
- Patients typically had pain for about 1 year that was worsened with athletic activity as well as sitting.
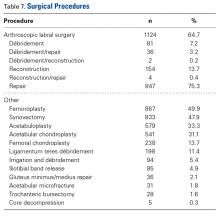
- The most common surgical procedures that were performed included labral surgery in 64.7%, femoroplasty in 49.9%, acetabuloplasty in 33.3%, and chondroplasty in 31.1%
Arthroscopic surgery of the hip has been growing over the past decade, with drastically increasing rates of arthroscopic hip procedures and increased education and interest in orthopedic trainees.1-3 The rise of this minimally invasive surgical technique may be attributed to expanding knowledge of surgical management of morphologic hip disorders as a means of hip preservation. Many arthroscopic techniques have been developed to treat intra-articular hip joint pathologies, including femoroacetabular impingement (FAI), labral tears, and cartilage damage.4-11 These hip pathologies are widely recognized as painful limitations to activities of daily living and sports as well as early indicators of hip osteoarthritis.12,13 Limited evidence suggests that arthroscopic treatment of these intra-articular hip joint pathologies preserves the hip from osteoarthritis and progression to total hip arthroplasty.13-15
FAI is the most common etiology of pathologies related to arthroscopic surgery of the hip, including both labral tears and cartilage damage.4,7,14 FAI is a morphologic bone disorder characterized by impingement of the femur and the acetabulum on flexion or rotation. The etiology of FAI is not completely understood, but evidence suggests that stress to the proximal femoral physis during skeletal growth increases the risk of developing femoral head and neck deformations leading to cam-type FAI.15-17 Understanding the characteristics of the patient population in which FAI occurs may shed light on the processes of intra-articular damage, such as labral tears and cartilage damage.
In the present study, we collected epidemiologic data, including demographics, pathologic entities treated, patient-reported measures of disease, and surgical treatment preferences, on a hip pathology population that elected to undergo arthroscopic surgery. These data are important in gaining a better understanding of the population and environment in which hip arthroscopy is performed across multiple centers throughout the United States and may help guide clinical practice and research to advance hip arthroscopy.
Methods
The Multicenter Arthroscopic Study of the Hip (MASH) Study Group conducts multicenter clinical studies in arthroscopic hip preservation surgery. Patients are enrolled in this large prospective longitudinal study at 10 sites nationwide by 10 fellowship-trained hip arthroscopists. Institutional Review Board approval was obtained from all institutions before patient enrollment. After enrollment, we collected comprehensive patient data, including demographics, common symptoms and their duration, provocative activities, patient-reported outcome measures (modified Harris Hip Score, International Hip Outcome Tool, 12-item Short Form Health Survey, visual analog scale pain rating, Hip Outcome Score), physical examination findings, imaging findings, diagnoses, surgical findings, and surgical procedures.
All study participants were patients undergoing arthroscopic hip surgery by one of the members of the MASH Study Group. Patients with incomplete preoperative information (needed for data analysis) were excluded. Data analysis was performed with SPSS Statistics Version 21.0 (SPSS Inc.) to obtain descriptive statistics of the quantitative data and frequencies of the nominal data.
Results
Between January 2014 and November 2016, we enrolled 1738 patients (647 male, 1091 female) in the study. Table 1 lists the demographics of the population.
Mean age was 34.6 years (range, 11-77 years); mean height, 67.1 inches (range, 54-180 inches); mean weight, 163.4 pounds (range, 62-325 pounds); and mean body mass index, 25.9 kg/m2 (range, 7-57.1 kg/m2). Ninety-seven percent of the patients were white, 1.7% African-American, 1% Hispanic, and 0.30% Asian. In 55% of the cases, the right side was involved; in 43%, the left side; and in 2%, both sides. Only 1.2% of patients reported being a smoker, and 1.1% had services paid through worker’s compensation claims.Regarding symptom location, 40.9% of patients described pain in the groin region, 24.2% in the anterior hip region, and 11.3% in a C-sign distribution (Table 2).
Lateral pain was reported by 17.6% of patients, and 13.8% of patients complained of pain in the posterior hip and buttock region. Figure 1 shows that, before surgery, symptoms lasted more than 2 years in 38.4% of cases, between 1 and 2 years in 22%, between 4 and 12 months in 28.7%, and less than 4 months in 10.9%. Figure 2 shows that symptoms were provoked during sports in 47.1% of cases, while sitting in 46.8%, while walking in 39.5%, while standing in 26.4%, and while climbing stairs in 19%. In addition, 22.3% of patients had a detectable limp, and catching, clicking, or locking occurred in 23.4% of patients.Table 3 lists the results of the patient-reported outcome measures.
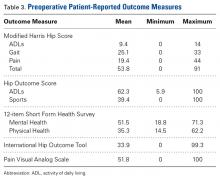
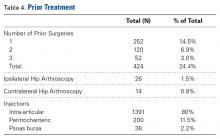
Mean visual analog scale pain rating was 51.8 (range, 0-100), mean modified Harris Hip Score was 53.8 (range, 0-91), mean Hip Outcome Score for activities of daily living was 62.3 (range, 5.9-100), mean Hip Outcome Score for sports was 39.4 (range, 0-100), and mean International Hip Outcome Tool was 33.9 (range, 0-99.3).Of the 1738 patients enrolled, 424 (24.4%) had prior surgery related to current symptoms, 252 (14.5%) had 1 previous surgery, 120 (6.9%) had 2 previous surgeries, and 52 (3%) had 3 previous surgeries. Twenty-six patients (1.5%) had a previous revision hip arthroscopy on the ipsilateral side, and 14 (0.8%) had a previous hip arthroscopy on the contralateral side. Before surgery, 80% of patients received an intra-articular injection of corticosteroid and lidocaine. The peritrochanteric region was injected in 11.5% of patients and the psoas bursa in 2.2% (Table 4).
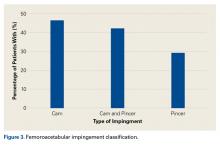
Eighty percent of patients attended physical therapy for their hip before electing to have surgery.Of the 1011 patients who had magnetic resonance imaging (MRI) performed, 943 (93.3%) had abnormal acetabular labrum findings, and 163 (17.1%) had acetabular articular damage. According to radiographic evaluation, 953 patients had abnormal hip joint morphology consistent with FAI. Figure 3 shows the FAI classification percentages.
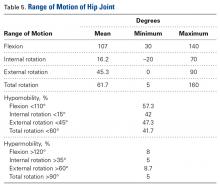
The combination of cam-type and pincer-type impingement was noted in 42.6% of cases, isolated cam-type impingement in 47%, and isolated pincer-type impingement in 29.5% (61 of the 107 isolated pincer cases had positive radiographic signs of focal acetabular overcoverage). Conversely, 84 patients (4.8%) had signs of hip dysplasia (lateral center edge angle, <25°). Of all 1738 patients, 1602 (92.5%) had Tönnis grade 0 osteoarthritis on radiographic evaluation, 6.3% had Tönnis grade 1, and 1.5% had Tönnis grade 2. The lateral joint space was the most common location for arthrosis (2.1%), followed by the medial joint space (1.3%) and the central joint space (1.1%).On clinical examination, 1079 patients (62.1%) had a positive anterior impingement sign. The subspine impingement sign was positive in 447 patients (25.7%), and the trochanteric pain sign was positive in 400 (23%). Table 5 lists range-of-motion values for flexion and hip rotation from 90° of flexion.
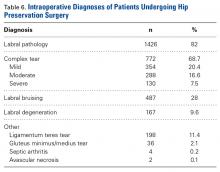
Loss of motion for hip flexion (<110°) occurred in 57.3% of patients, hip internal rotation of <15° in 42%, external rotation of <45° in 47.3%, and total hip rotation of <60° in 41.7%.As seen in Table 6, labral pathology was the most common diagnosis (1426/1738 patients, 82%).
Of the entire population, 354 (20.4%) had mild complexity labral tears, 288 (16.6%) had moderate complexity labral tears, and 130 (7.5%) had severe complexity labral tears. Of the 1738 cases total, 487 (28%) had labral bruising, and 167 (9.6%) had degenerative tears. Other diagnoses were 4 cases of septic arthritis (0.2%), 2 cases of avascular necrosis (0.1%), 36 cases of gluteus minimus/medius tears (2.1%), and 198 ligamentum teres tears (11.4%).As seen in Table 7, the most common procedure was femoroplasty (867/1738, 49.9%).
Other common procedures were synovectomy (833, 47.9%), acetabuloplasty (579, 33.3%), and acetabular chondroplasty (541, 31.1%). Of the 1124 labral tears, 847 (75.3%) were repaired, 154 (13.7%) were reconstructed, and 81 (7.2%) were débrided.