Those are key conclusions from a consensus statement based on a systematic review of existing evidence in the medical literature about ventral hernia management that were published in the January 2017 issue of the Annals of Surgery.
“Despite ventral hernias (VH) being one of the most common pathologies seen by clinicians, significant variability in management exists,” wrote the researchers, led by Mike K. Liang, MD, of the University of Texas Health Science Center at Houston. “Surveys of clinicians and review of nationwide databases of patients undergoing elective ventral hernia repair (VHR) demonstrate substantial heterogeneity in patient selection and clinical practice.”
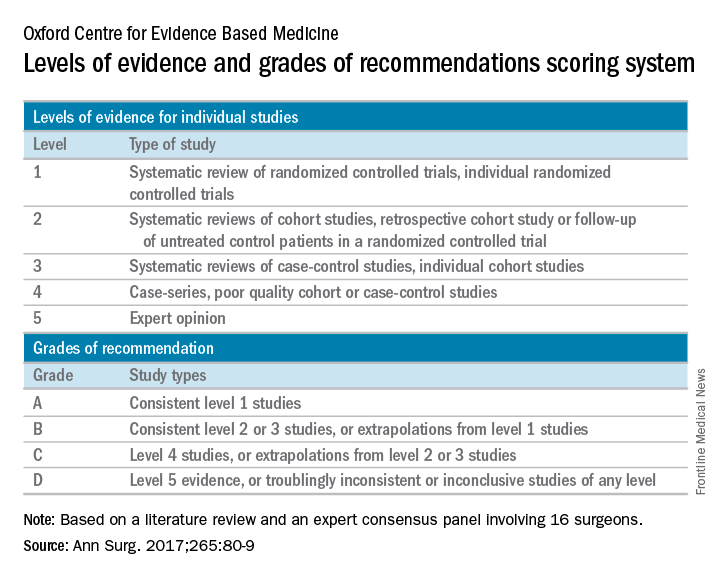
In an effort to achieve consensus regarding best practices in managing VH, a panel of 16 expert hernia surgeons convened to identify the highest level of evidence available on patient selection, preoperative optimization, nonoperative management, and intraoperative decision making gleaned from articles published from Jan. 1, 1980, to May 1, 2015, and to reach consensus on those topics (Ann Surg. 2017;265:80-9). The data consisted of reviews, meta-analyses, randomized trials, cohort studies, and case series that were assigned a level of evidence score and a grade of recommendation from A (“consistent level 1 studies”) to D (“troublingly inconsistent or inconclusive studies of any level”). Of the 16 panel members, 13 were in academic practice and 3 were in private practice.The panelists agreed that complications with VHR increase in obese patients (grade A evidence), current smokers (grade A), and in patients with glycosylated hemoglobin A1c (HbA1c) of 6.5% or greater (grade B). They did not recommend elective VHR in patients with a body mass index of 50 kg/m2 or greater (grade C), in current smokers (grade A), or patients with an HbA1c of 8.0% or greater (grade B). They also agreed that patients with a BMI of 30-50 kg/m2 or an HbA1c level of 6.5%-8.0% require individualized interventions to reduce surgical risk (grade C, grade B, respectively). The panelists considered nonoperative management to have a low risk of short-term morbidity (grade C) and they recommended mesh reinforcement for repair of hernias 2 cm or greater in size (grade A).
The panelists failed to reach agreement on several areas where high-quality data were limited, including mesh type. “Categories include ultra-light weight, light-weight, mid-weight, heavy-weight, and super-heavy weight, though precise definitions for each category are variable,” authors of the consensus statement wrote. “Randomized controlled trials are needed to compare synthetic, biological, and bioabsorbable meshes in all VH types and clinical settings.”
Data were also insufficient to recommend one type component separation technique over another. “Existing studies compare anterior component separation with another technique (e.g., perforator sparing, endoscopic, or posterior) and all have demonstrated that anterior component separation has the highest rate of wound complications,” the authors wrote. “Although some members of the consensus panel stated they prefer posterior component separation (8/16, 50%), concerns were expressed over the limited long-term data on the safety of this approach.”The authors of the consensus statement also called for further high-quality studies to better assess the management of VH in complex patients, which they defined as those presenting acutely, patients with cirrhosis, patients with inflammatory bowel disease, and patients who are pregnant.
The authors acknowledged certain limitations of the statement, including the fact that not all VH experts were included on the consensus panel. “However, the panel consisted of a large group of national experts with a primary practice focus of VHR,” they wrote. “The panelists have diverse views and unique areas of knowledge in the realm of hernia repair. The differing backgrounds among panelists was intended to make the guidelines that were developed more generalizable, as there is a wide variety of experience and skill level in the surgical community. In addition, there are no objective criteria to define an ‘expert’ in VH management.”
This work was supported by the Center for Clinical and Translational Sciences. The authors reported having no financial disclosures.