Take-Home Points
- Use ultrasound to identify integrity and location of MPFL tear.
- Anatomic repair allows native tissue to reintegrate into bone.
- Repairs done early can prevent complications of recurrent instability.
- Repair maintains biological and proprioceptive qualities of tissue.
- 10Ultrasound-guided percutaneous repair is quick and effective.
The medial patellofemoral ligament (MPFL) is the primary passive restraint to lateral patellar excursion1-5 and helps control patellar tilt and rotation.6,7 More than 90% of lateral patellar dislocations cause the MPFL to rupture, and roughly 90% of these detachments involve the femoral insertion.4 Ensuing patellar instability often results from MPFL insufficiency. It has been suggested that re-creating the anatomy and functionality of this ligament is of utmost importance in restoring normal patellar biomechanics.1-5,7,8
Anatomical risk factors for recurrent patellar instability include patella alta, increased tibial tuberosity-trochlear groove (TT-TG) distance, trochlear dysplasia, and torsional abnormalities.1-4,6 A medial reefing technique with a lateral tissue release traditionally was used to restore proper kinematics, but was shown to have associated postoperative issues.9
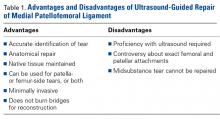
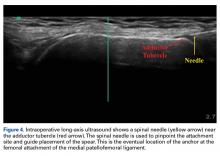
In recent years, ligamentous reconstruction has become the gold standard for surgical intervention.6-8 The precise location of the MPFL attachments, particularly at the femoral insertion, has been the subject of a great deal of debate. McCarthy and colleagues10 suggested that the anatomical location at the femur is just anterior and distal to the adductor tubercle, but they noted that determining this location during surgery is difficult. Use of fluoroscopy has become the gold standard for identifying proper tunnel placement for reconstruction.10,11 However, the inability of fluoroscopy to consistently identify the anatomical MPFL attachments has proved to be a shortcoming of this technique.11,12In this article, we present a novel technique for percutaneous repair of patella- or femur-side MPFL tears. It is performed with ultrasound guidance, which allows accurate identification of anatomy before and after surgery (Figures 1-3). Ultrasound has several advantages over other techniques and has not been described in other published works on MPFL procedures (Table 1).Methods
Patient Demographics
Dr. Hirahara developed this technique in 2013 and performed it 11 times between 2013 and 2016. Of the 11 patients, 1 was excluded from our retrospective analysis because of trochlear dysplasia, now considered a relative contraindication. Of the remaining 10 patients, 5 (50%) had the repair performed on the right knee. Eight patients (80%) were female. Mean (SD) age was 17.21 (3.53) years. One patient had concurrent femur- and patella-side detachments; otherwise, 6 (60%) of 10 repairs were performed exclusively at the patella. We grade patellar instability according to amount of glide based on patellar width and quadrants. Normal lateral displacement was usually 1 to 2 quadrants of lateral glide relative to the contralateral side. Before surgery, 6 (60%) of the 10 patients presented with lateral glide of 3 quadrants, and 3 (30%) presented with lateral glide of 4 quadrants. All had patellar instability apprehension on physical examination.
Surgical Indications
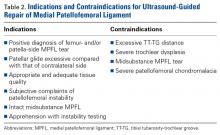
Before surgery, MPFL integrity is determined by ultrasound evaluation. Repair is considered if the MPFL has a femur- or patella-side tear and is of adequate quantity and quality, and if there are minimal or no arthritic changes (Table 2).
As the MPFL is the main constraint to lateral patellar displacement, patients continue to have excessive patellar instability if left insufficient.Surgical Technique
The patient is brought to the operating room and placed supine. Patellar stability of the affected knee is assessed and compared with that of the contralateral side with patellar glide. The knee is prepared and draped in usual sterile fashion. With the knee flexed at 90º, a tourniquet is inflated. Diagnostic arthroscopy is performed with standard anteromedial and anterolateral portals, and, if necessary, arthroscopic procedures are performed.
Femoral Attachment Repair
With the leg in extension, ultrasound is used to identify the tear at the femoral attachment (watch part 1 of the video). A spinal needle is placed at the femoral insertion, typically just anterior and distal to the adductor tubercle (Figure 4).10 A scalpel is used to make a 1-cm incision through the tissue and down to the attachment. The area is débrided and abraded. A drill is used to create an appropriate socket, and a 3.0-mm suture anchor (BioComposite Knotless SutureTak; Arthrex) is placed into the attachment site. A suture passer (Labral FastPass Scorpion; Arthrex) is used to pass the sutures through the leading edge of the torn MPFL in horizontal mattress fashion and tie it to the anchor, completing the repair. Lateral glide and range of motion (ROM) are tested to ensure adequate tensioning, and ultrasound can be used to corroborate proper anchor placement.