BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
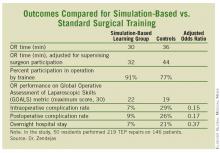
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.