The study, done at 26 U.S. centers, found that at 6 and 12 months after treatment, 54 patients who received the low-dose injections had significantly fewer angina episodes per week than the 53 patients who received placebo infections, the study’s primary end point. Patients who received the higher-dose injections also had fewer angina episodes than the controls, but the difference was not statistically significant at either 6- or 12-month follow-up. The low-dose patients also had statistically significant improvement in their total exercise time in an exercise tolerance test compared with the placebo patients; the high-dose patients also had better exercise times, but not significantly better than the controls.
Speaking at the American College of Cardiology meeting in Chicago in March, Dr. Losordo presented 2-year follow-up data on the patients in ACT34-CMI. At 2 years, the low-dose patients continued to have a significantly lower rate of weekly angina counts than control patients, while the high-dose patients continued to have a numerically lower rate that was not significantly different from the controls. The cumulative, 2-year rate of death, MI, or hospitalization for acute coronary syndrome was 30% in the control patients, 18% in the low-dose patients, and 14% in the high-dose patients. Although these between group differences were not statistically significant, the trends were "in the right direction," said Dr. Losordo, an interventional cardiologist at Northwestern University in Chicago, and vice president for new therapeutic development at Baxter International. Baxter sponsored ACT34-CMI, as well as the phase III study now starting based on the phase II results.
The phase III study, A Prospective, Randomized, Double-blinded, Active-control and Unblinded Standard of Care (SOC) Controlled Study to Determine the Efficacy and Safety of Targeted Intramyocardial Delivery of Autologous CD34+ Cells (Auto-CD34+ Cells) for Increasing Exercise Capacity During Standardized Exercise Testing in Subjects With Refractory Angina Pectoris and Chronic Myocardial Ischemia (RENEW), will enroll about 450 refractory angina patients at 50 U.S. sites, randomizing them to CD34+ treatment, placebo treatment, or no treatment and optimal standard care. The primary efficacy outcome will be change in total exercise time on an exercise tolerance test after 12 months.
Choosing the Right Cells
The success of the ACT34-CMI study, and the decision by Dr. Losordo and Baxter to move on to the phase III RENEW trial, highlights what may be a possible advantage to using selected stem and progenitor cells compared with the strategy of using an unselected cell population, such as the bone-marrow cells used in many of the studies of the past 11 years.
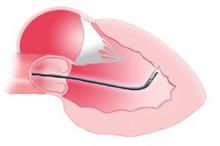
More evidence favoring cell selection came recently in results reported by Dr. Perin from the First Mononuclear Cells Injected in the United States Conducted by the Cardiovascular Cell Therapy Research Network (FOCUS-CCTRN) study, which he presented in March at the American College of Cardiology meeting in Chicago. The phase II study enrolled 92 patients with chronic heart failure and a left ventricular ejection fraction of 45% or less. Patients received a transendocardial injection of 100 million autologous bone-marrow cells or placebo. The primary end points were 6-month changes in left ventricular end systolic volume, in maximal oxygen consumption, and the extent of ischemic myocardial defects measured by single photon emission tomography. The results showed no statistically significant improvement for any of these three end points in the patients treated with bone-marrow cells compared with the controls, and were simultaneously reported in an article published online (JAMA 2012; March 24 [doi:10.1001/jama.2012.418]).
Despite the study’s failure for its prespecified end points, it also showed signals of efficacy and possibly highlighted some important lessons on how to best apply stem cell therapy in the future. On the efficacy side, the 61 patients who received bone-marrow cell injections had an average 1.4% improvement in their left ventricular ejection fraction, compared with an average 1.3% decline in the 31 placebo patients, an overall between-group difference of 2.7% that was statistically significant. Further analysis showed that patients who received bone-marrow cell preparations that had higher levels of either CD34+ cell or CD133+ cells had greater increases in their left ventricular ejection fractions. Also, when the researchers analyzed responses in subgroups divided by their age, patients 62 years old or younger (62 years old was the median age in the study) who received bone-marrow cells had a statistically significant, 4.7% improvement in their left ventricular ejection fraction after 6 months compared with placebo patients, while among patients greater than 62 years old treatment with autologous bone-marrow cells produced no significant improvement in ejection fraction compared with the controls.