Frequent rotations offer a valid means to foster leadership skills much needed in a military conflict zone and maximize military professional development; however, rotations also contribute to the lack of continuity of patient care. This PCM instability and the distinctive military dynamic volatility are characteristic of standard military operating procedure and are unlikely to change.
New solutions are needed to promote improved continuity of care for patients with diabetes at a MEDCEN. According to Lt Gen Eric Schoomaker, former Surgeon General of the Army, “The Patient-Centered Medical Home concept is being adopted throughout the military health system.”14 The goal of the trend toward patient-centered medical home (PCMH) care delivery is to improve access to high-quality health care services.13
Patient-Centered Medical Home
The term patient-centered medical home was introduced in 1967 by the American Academy of Pediatrics (AAP).15 In 2008, PCMH principles became integral in most health care reform initiatives.16 In most PCMH models, increased continuity of care is the single common denominator of practice. Continuity of care is defined as intensified integration, coordination, and sharing of information between disciplines that result in improved patient outcomes.10,17,18
In 2007, a consensus statement was provided by the American Academy of Family Practice, the AAP, American College of Physicians, and the American Osteopathic Association stating that quality and safety are hallmarks of the PCMH and may improve outcomes for chronic disease, such as diabetes.19
Quality improvement is vital in health care organizations because of demands by government agencies, health maintenance organizations, and the public to continually improve services and to provide the highest quality health care at the best cost.20 Diabetes has become a public health crisis, as previously discussed, and a comprehensive approach to care management is essential. Developing an optimal process for diabetes health care and methods for evaluation of the delivery process is foundational for all stakeholders involved, including health care organizations, health care providers, and patients.20
Diabetic outcomes were evaluated at a recent 2-year trial PCMH approach T2DM clinic at a MEDCEN at WBAMC. The purpose of the project was to determine whether a PCMH approach improves disease management compared with routine primary care management.
Methods
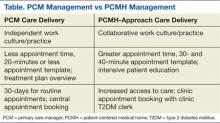
The process and manner of care delivery was the focus of this analysis and evaluation, not clinician knowledge of treatment management. A comparison of care delivery approaches of PCM management and PCMH care delivery is displayed in the Table. The treatment algorithm for T2DM was not in question, because guidelines for practice are established based on scientific evidence, and medication management is based on evidence-based practice.21,22 Evaluation consisted of T2DM delivery of care process and the efficacy of outcome achieved by the specified delivery of care: (a) increased access to care; (b) intensive, repeated education; and (3) a multidisciplinary approach focused on patient empowerment. The following is a description of the specified delivery of care.
Increased Access to Care
Increased access to care addressed through frequent telecommunication provided by the registered nurse (RN) case manager who regularly called patients within 72 hours of insulin adjustment or 24 hours for insulin initiation or significant medication changes. Additionally, the diabetes team providers requested a follow-up appointment in 1 week when injectable medication was added or changes were made in insulin management. One exception was for the addition of livaglutide, in which a 2-week follow-up was made, to allow for titration of the medication. For oral medication adjustment, a 1-month follow-up was generally made, with a 2-month follow-up when a glucose histogram indicated optimal glycemic control, an average blood glucose of 7% (estimated average glucose of 154 mg/dL) or less. Time for appointments was increased by 10 minutes for a total of 30-minute appointments, compared with 20 minutes for PCM delivery.
Informational continuity was thought to be improved by use of an electronic medical record (EMR), allowing for an uninterrupted patient record. Providers were expected to document medication reconciliation with a clear explanation of medication adjustments listed in the plan. Patient teaching was documented, describing the specific patient education concerns addressed. Other data included a glucometer statistical report from the last appointment to the current appointment, to track negative or positive changes in glycemic control.
Patient Education
The management technique used in the clinic was intensive, repeated education with the goal of improving learning and retention with repeated instruction and positive reinforcement. Skinner theorized that learning is the acquisition of new behavior through conditioning (eg, repeated instruction), is in close proximity of time, and is likely to result in learning retention, which remain relevant education practice.23,24 The T2DM clinic operates on Skinner’s principles of repeated, intensive education. For example, patients must bring their glucometer to every appointment. The statistical analysis downloaded from the glucometer provides immediate reinforcement and information about patients’ glycemic control. Patients are typically excited to see an improvement from previous levels and are encouraged to continue behavior modification. Conversely, statistical analysis demonstrating poor glycemic control generally encourages the patient to make needed lifestyle changes. Thus, changes in behavior due to intensive, repeated education, followed by a reinforcing stimulus results in an increased probability of that behavior occurring in the future.23,25 The interdisciplinary team provides education during each T2DM patient encounter.