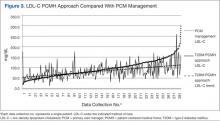
Low-density lipoprotein cholesterol levels were analyzed to determine whether patients with diabetes managed at the WBAMC T2DM clinic also had improved lipid control. A total of 638 patients had an initial LDL-C level drawn prior to clinic management. Of these patients, 282 were acceptable for analysis (Figure 2). Low-density lipoprotein cholesterol data were omitted because 93 did not have a paired pre- and postvalues, 8 values were invalid due to nonfasting laboratory status; and 255 values were omitted due to having < 2 clinic visits. Results of the data analysis demonstrated that LDL-C was well managed by the T2DM clinic, with levels ≤ 100 mg/dL (P < .001) (Figure 3).
Discussion
The WBAMC T2DM clinic was formed as a trial clinic at a medical treatment facility (MTF) MEDCEN due to the failure of routine PCM care to improve outcomes in the management of the diabetes population (A1c < 7.0%). Overall, improved endpoints of A1c, LDL-C were achieved with the disease-specific PCMH approach compared with routine PCM approach. The results indicate that disease-specific management leads to improved diabetic endpoints (A1c reduction by at least 1% and LDL-C < 100 mg/dL). The clinic’s protocol (listed in the methods) was intended to improve continuity.
A review of the literature confirmed that continuity of care is integral to patient satisfaction and improved diabetes management.8,10,17,28,29 The results of the study were consistent with those in the literature. The review of the literature established that patients who develop a trusting relationship with the health care provider as the T2DM clinic promoted (eg, frequent patient appointments, telecommunication by nurse, and patient participation) are more likely to follow medical therapy and take a proactive role in disease management.6,28,30
Conclusion
This study demonstrated that PCMH-delivered care offers a solution to suboptimal management of chronic disease, such as T2DM, and that chronic disease is best managed by implementation of a disease-specific PCMH. It is recommended that a MTF develop other disease-specific PCMH and pilot-test these programs. Long-term follow-up studies and additional data collection, such as blood pressure control, abdominal circumference, body mass index, and triglyceride levels would be useful to determine effectiveness.
Based on principles of a PCMH, the efficacy of the T2DM clinic at WBAMC demonstrated that improved diabetes management was achieved by increased continuity of care; intensive, repeated patient education; and a multidisciplinary team approach. The CDC identifies self-management training as foundational to improving health outcomes and QOL for individuals with diabetes.1 Primary care providers in a MTF may improve diabetic patient outcomes by referring patients to a T2DM clinic, such as the WBAMC T2DM clinic. The multidisciplinary team facilitated patient empowerment by educating patients on the management of their disease and the problem-solving and coping skills required to manage a chronic disease.
The WBAMC T2DM-PCMH based mission of fostering patient empowerment and a team approach is a comprehensive approach to diabetes care. Currently, the PCMH model is being adapted by the military in the latest health care reform initiatives.14 However, the move toward the PCMH model does not incorporate disease-specific PCMH clinics. This study demonstrates that the disease-specific PCMH approach provides improved disease management and may be effective in other chronic disease management. A benefit of the T2DM-PCMH approach is the reduced burden of escalating health care costs related to increased morbidity and mortality, which is associated with the growing health care problem of poorly controlled T2DM.1,4,31
The disease-specific clinic evaluated at WBAMC provides an effective solution to fragmented health care for the optimal management of T2DM. The clinic’s conceptual framework of increased access to care, with consistent education at closer time intervals when compared with PCM management resulted in improved continuity and T2DM control. Future research in this area should assess measurable cost reduction. Improved disease management as demonstrated by the T2DM disease-specific clinic at WBAMC provides sufficient incentive to incorporate similar T2DM continuity clinics and changes throughout MTFs.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.