NEW YORK – Despite initial concerns that stopping tyrosine kinase inhibitor treatment would be ill-advised in patients with chronic myeloid leukemia (CML), clinical trial data suggest it is a safe and reasonable strategy, according to a leading expert.
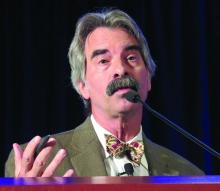
“About 95% of people in all of these trials will regain their original response when they start off on therapy again,” said Jerald P. Radich, MD, of Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance.
“There’s been a few that don’t, but blast crisis has been very, very rare, thank goodness, so it looks to be fairly safe for now,” Dr. Radich said at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
That being said, careful follow up is still required, Dr. Radich cautioned, noting that there was still an excess of CML in Hiroshima and Nagasaki atomic bomb survivors evident decades after radiation exposure.
“CML is a very strange disease,” he said. “You can’t eliminate the possibility of some slow-growing clone that, once you take [a patient] off tyrosine kinase therapy, is going into an accelerated phase and might take years to manifest itself.”
In one of the latest reports to shed light on what happens after discontinuation, investigators for the ENESTop study reported that treatment-free remission “seems achievable” in patients who have sustained, deep remissions after discontinuing nilotinib second-line therapy (Ann Intern Med. 2018 Apr 3;168[7]:461-70).
In ENESTop, chronic phase CML patients on tyrosine kinase inhibitors for at least 3 years were eligible to discontinue therapy if they achieved MR4.5 (BCR-ABL1IS of 0.0032% or less) and maintained that response level during a 1-year consolidation phase.
Out of 163 patients in the study, 126 met the criteria to enter the treatment-free remission phase; of that subset, 58% maintained treatment-free remission at 48 weeks, while 53% maintained it at 96 weeks, investigators said.
For 56 patients who restarted nilotinib, 55 regained at least major molecular response (MMR), and 52 regained MR4.5, while none had progression to accelerated phase or blast crisis, according to the report.
Similarly, earlier reported results from the ENESTfreedom trial showed that, of 190 patients entering the treatment-free remission phase after a median duration of 43.5 months on nilotinib, more than half remained in MMR or better at 48 weeks (Leukemia. 2017 Jul;31[7]:1525-31).
Of 86 patients who started nilotinib again after losing MMR, 98.8% regained MMR and 88.4% regained MR4.5 by the data cutoff date for the trial.
Duration and depth of response may make a “little bit of difference” in likelihood of relapse, Dr. Radich added.
In an interim analysis of a prospective multicenter, nonrandomized European discontinuation trial (EURO-SKI), investigators found that patients achieving deep molecular responses had good molecular relapse-free survival (Lancet Oncol. 2018 Jun;19[6]:747-57).
Based on that, investigators suggested that patients with deep molecular responses should be considered for discontinuation to spare them from side effects and to reduce health expenditures.
Results of these and other trials are “pretty much unbelievable,” Dr. Radich said. That’s in part because mathematical modeling – extrapolated from early trials – had suggested it could take nearly 50 years to completely eradicate minimal residual disease with tyrosine kinase inhibitors, and that the cumulative cure rate after 30 years of treatment could be as low as 31%.
Dr. Radich reported financial disclosures related to Amgen, Novartis, and Seattle Genetics.