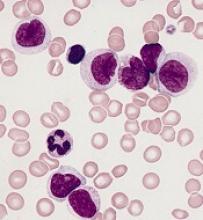
Next-generation sequencing (NGS) can be used to predict relapse in acute myeloid leukemia (AML) patients undergoing hematopoietic stem cell transplant (HSCT), according to research published in Blood.
Researchers found that patients with a higher variant allele frequency (VAF) 21 days after HSCT had a higher risk of relapse and death.
“We can detect mutations in patients’ bone marrow cells 3 weeks after the transplant and, based on that, predict the likelihood of their relapse,” explained study author Zhaolei Zhang, PhD, of the University of Toronto in Ontario, Canada.
Dr. Zhang and his colleagues performed NGS on 529 bone marrow samples from 104 AML patients who underwent chemotherapy and HSCT.
The samples were collected at the time of diagnosis, during the chemotherapy-induced remission, and 3 weeks after HSCT. A subset of patients also gave samples at 3 months, 6 months, and 12 months after HSCT.
The researchers identified 256 mutations that were present in 90 patients at diagnosis and looked for those same mutations at each sampling point.
Chemotherapy and HSCT eliminated most AML cells, leading to a reduction in mutation frequency. However, in some patients, mutations observed at diagnosis could still be detected after chemotherapy and at day 21 after HSCT, indicating the presence of treatment-resistant AML cells.
Allelic burdens at day 21 post-HSCT were higher in patients who ultimately relapsed, and the mutations observed at day 21 expanded at relapse.
The 3-year relapse rate was 56.2% in patients with a VAF greater than 0.2% at day 21 post-HSCT, compared to 16.0% in patients with a lower or no mutational burden (P<0.001).
The 3-year overall survival rates were 36.5% in patients with a VAF greater than 0.2% and 67.0% for patients with a lower or no mutational burden (P=0.006).
In multivariate analyses, VAF0.2% at day 21 was an independent adverse prognostic factor for relapse—hazard ratio, 4.75 (P<0.001)—and overall survival—hazard ratio, 3.07 (P=0.003).
Dr. Zhang and his colleagues said these results suggest NGS-based monitoring after HSCT “provides valuable information” that, together with a patient’s baseline mutational profile and clinical evaluation, can be used to predict outcomes of transplant.
This study was supported by research grants from the Natural Science and Engineering Council of Canada, Leukemia and Lymphoma Society of Canada, Princess Margaret Foundation, National Research Foundation of Korea, and National Natural Science Foundation of China.