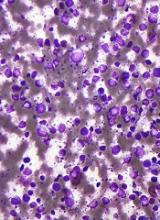
New research helps explain why some patients with diffuse large B-cell lymphoma (DLBCL) respond well to immunochemotherapy and others do not.
Researchers analyzed samples from nearly 600 DLBCL patients and identified 4 new genetic subtypes of the disease.
Patients with 2 of these subtypes had overall survival (OS) rates that were roughly twice as high as OS rates in patients with the other 2 subtypes.
Louis M. Staudt, MD, PhD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues described these findings in NEJM.
The researchers noted that the current subtypes of DLBCL—germinal center B-cell-like (GCB) and activated B-cell-like (ABC) DLBCL—are associated with OS after treatment with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
Patients with ABC DLBCL have a much lower OS rate, on average, than patients with GCB DLBCL. However, even in the GCB subgroup, many patients relapse after treatment.
“The first question we wanted to tackle was whether there were other molecular features of the tumors that could help us explain why some people were well-served by chemotherapy,” Dr Staudt said.
“And the second, related question was, if we could understand who was not responding well to treatment, could we understand the genetics of these tumors to suggest new potential therapies beyond chemotherapy? The answer to both questions was ‘yes.’”
Dr Staudt and his colleagues analyzed tumor samples from 574 patients with DLBCL, performing exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes to find recurrent aberrations.
The team also developed an algorithm to discover genetic subtypes based on the co-occurrence of genetic alterations.
In this way, they identified 4 genetic subtypes:
- MCD, which was named based on the co-occurrence of MYD88L265P and CD79B mutations
- BN2, whose name was based on the presence of BCL6 fusions and NOTCH2 mutations
- N1, named for NOTCH1 mutations
- EZB, named for EZH2 mutations and BCL2 translocations.
The researchers said aberrations in multiple genes distinguished each of these subtypes from other DLBCLs, and the subtypes differed phenotypically.
Patients with BN2 or EZB subtypes had much higher OS rates after receiving R-CHOP than patients with MCD or N1 subtypes. The predicted 5-year OS rates were 26% for MCD patients, 36% for N1 patients, 65% for BN2 patients, and 68% for EZB patients.
The researchers said they found evidence to suggest that MCD and BN2 DLBCLs rely on chronic active B-cell receptor signaling that is amenable to therapeutic inhibition.
The team also noted that some of the subtypes they identified can be found in both ABC and GCB DLBCLs. For example, a patient could have ABC DLBCL, which is associated with a lower OS rate after R-CHOP, but also have the BN2 genetic subtype that responds well to R-CHOP.
“This shows we’ve gone beyond where we were,” Dr Staudt said. “Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type, and they need to be treated aggressively.”
“Now, we can implement this kind of classification and say that, even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
Data from this study will be shared through the National Cancer Institute’s Genomic Data Commons to make it available for future research.
Dr Staudt said he and his colleagues hope their new molecular classification will be used in clinical trials so that DLBCL treatment can move toward more targeted therapies.
“The goal is to find the right drug for the right person at the right time,” Dr Staudt said. “And we feel this genetic understanding of diffuse lymphoma is a step forward in precision therapy.”