Rigosertib has demonstrated activity and tolerability in patients with myelodysplastic syndromes (MDS) and acute myeloid leukemia transformed from MDS (tAML), according to researchers.
In a phase 1/2 study, rigosertib produced responses in a quarter of MDS/tAML patients and enabled stable disease in another quarter.
Overall survival (OS) was about a year longer for responders than for non-responders.
MDS patients were more likely to respond to rigosertib and therefore enjoyed longer OS than tAML patients.
Overall, rigosertib was considered well-tolerated. There were no treatment-related deaths, though 18% of patients experienced treatment-related serious adverse events (AEs).
Lewis Silverman, MD, of Icahn School of Medicine at Mount Sinai in New York, New York, and his colleagues described these results in Leukemia Research.
The study was sponsored by Onconova Therapeutics, Inc., the company developing rigosertib.
Rigosertib is an inhibitor of Ras-effector pathways that interacts with the Ras binding domains common to several signaling proteins, including Raf and PI3 kinase.
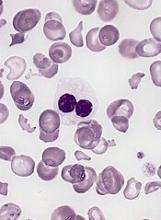
Dr Silverman and his colleagues tested intravenous rigosertib in a dose-escalation, phase 1/2 study of 22 patients. Patients had tAML (n=13), high-risk MDS (n=6), intermediate-2-risk MDS (n=2), or chronic myelomonocytic leukemia (n=1).
All patients had relapsed or were refractory to standard therapy and had no approved options for second-line therapies. The patients’ median age was 78 (range, 59-84), and 90% were male.
Patients received 3- to 7-day continuous infusions of rigosertib at doses ranging from 650 mg/m2/day to 1700 mg/m2/day in 14-day cycles.
The mean number of treatment cycles was 5.6 ± 5.8 (range, 1-23). The maximum tolerated dose of rigosertib was 1700 mg/m2/day, and the recommended phase 2 dose was 1375 mg/m2/day.
Safety
All patients had at least 1 AE. The most common AEs of any grade were fatigue (n=16, 73%), diarrhea (n=12, 55%), pyrexia (n=12, 55%), dyspnea (n=11, 50%), insomnia (n=11, 50%), anemia (n=10, 46%), constipation (n=9, 41%), nausea (n=9, 41%), cough (n=9, 41%), and decreased appetite (n=9, 41%).
The most common grade 3 or higher AEs were anemia (n=9, 41%), thrombocytopenia (n=5, 23%), pneumonia (n=5, 23%), hypoglycemia (n=4, 18%), hyponatremia (n=4, 18%), and hypophosphatemia (n=4, 18%).
Four patients (18%) had treatment-related serious AEs. This included hematuria and pollakiuria (n=1), dysuria and pollakiuria (n=1), asthenia (n=1), and dyspnea (n=1). Thirteen patients (59%) stopped treatment due to AEs.
Ten patients, who remained on study from 1 to 19 months, died within 30 days of stopping rigosertib. There were no treatment-related deaths.
Efficacy
Nineteen patients were evaluable for efficacy.
Five patients responded to treatment. Four patients with MDS had a marrow complete response, and 1 with tAML had a marrow partial response. Two of the patients with marrow complete response also had hematologic improvements.
Five patients had stable disease, 3 with MDS and 2 with tAML.
The median OS was 15.7 months for responders and 2.0 months for non-responders (P=0.0070). The median OS was 12.0 months for MDS patients and 2.0 months for tAML patients (P<0.0001).
“The publication of results from this historical study provides support of the relationship between bone marrow blast response and improvement in overall survival in this group of patients with MDS and acute myeloid leukemia for whom no FDA-approved treatments are currently available,” said Ramesh Kumar, president and chief executive officer of Onconova Therapeutics, Inc.
He added that these data are “fundamental to the rationale” of ongoing studies of rigosertib in high-risk MDS patients.