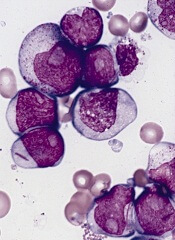
Results of preclinical research suggest the wild-type version of SYK pairs with mutated FLT3 to promote progression of acute myelogenous leukemia (AML).
And this molecular partnership promotes AML cells’ resistance to FLT3 inhibitors.
However, adding a SYK inhibitor to the mix can override this resistance. In an animal model of AML, treatment with a combination of FLT3 and SYK inhibitors was significantly more effective than either inhibitor alone.
These findings, published in Cancer Cell, raise hopes that treatment strategies focusing on both enzymes simultaneously could improve outcomes for patients with FLT3-ITD AML.
“Patients whose AML cells express FLT3-ITD are among the highest-risk group of patients with AML,” said study author Kimberly Stegmaier, MD, of the Dana-Farber Cancer Institute in Boston. “Their AML is particularly difficult to treat.”
In 2009, researchers in Dr Stegmaier’s lab discovered that SYK, a kinase that had attracted attention for its role in other malignancies, could be a potential drug target in AML. Unlike other cancer-associated kinases, SYK rarely undergoes mutations or other genomic alterations in cancer cells, remaining in its wild-type form.
With the current study, Dr Stegmaier and her colleagues set out to better understand SYK’s role in AML. The team screened AML cell lines to reveal the full scope of the enzyme’s molecular interactions. And they found evidence of strong interactions between wild-type SYK and mutated FLT3, particularly FLT3-ITD.
“We wanted to understand the cooperative oncologic effects by which SYK contributes to AML,” Dr Stegmaier said. “The concept of a normal enzyme aiding a mutant one has not yet been widely explored, and so we were both surprised and pleased to see FLT3-ITD come up as a high-priority hit in our screens.”
Through experiments in cell lines, primary patient samples, and animal models, the researchers found that SYK and FLT3-ITD’s interactions are a key ingredient in the progression of myeloproliferative neoplasms into AML. AML cells’ continued growth after turning malignant also relied on these interactions.
In addition, the team found that SYK’s hyperactivated form can promote resistance to the FLT3-targeting drug quizartinib. However, a combination of quizartinib and the SYK inhibitor PRT062607 overcame this resistance, significantly increasing survival and reducing signs of disease in a FLT3-ITD AML mouse model.
Highlighting their findings’ clinical relevance, the researchers found strong SYK activity in cells from FLT3-ITD AML patients. The cells were also highly sensitive to SYK inhibition.
“These data affirm that SYK is an important target in AML,” Dr Stegmaier said. “They also suggest that interactions between oncologic kinases and SYK or other wild-type enzymes may contribute to resistance of kinase inhibitors more broadly.”
Dr Stegmaier added that, over the course of this research, the team has developed a suite of tools that could prove useful for future clinical studies of treatments with SYK inhibitors or SYK inhibitors in combination with FLT3 inhibitors.
“We have not only identified SYK as a candidate treatment target in AML, but we have also identified a specific population of patients with AML more likely to respond to SYK inhibitors: patients with FLT3 mutations,” she said.
“Moreover, we have developed tools for identifying patients with high levels of SYK and FLT3 activation and can monitor these 2 targets while patients are receiving treatment. Predictive biomarkers of response are becoming increasingly important in the development of effective clinical trials of targeted therapies.”

