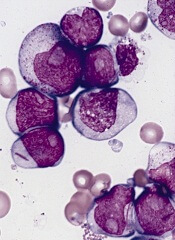
acute myeloid leukemia
SAN DIEGO—A next-generation DNA hypomethylating agent has demonstrated clinical activity and an acceptable safety profile in relapsed/refractory acute myeloid leukemia (AML), according to researchers.
The agent, guadecitabine, produced a composite complete response (CRc) rate of 23% in a phase 2 study.
CRc was observed in all patient subgroups and was associated with longer survival, regardless of whether patients went on to receive a transplant.
Based on these results, researchers are initiating a phase 3 trial of the drug in relapsed/refractory AML.
Naval Daver, MD, of the University of Texas MD Anderson Cancer Center in Houston, presented the phase 2 results at the 2016 ASH Annual Meeting (abstract 904). The study was sponsored by Astex Pharmaceuticals.
Guadecitabine (formerly SGI-110) is a hypomethylating dinucleotide of decitabine and deoxyguanosine that is resistant to cytidine deaminase degradation. It is administered as a small volume subcutaneous injection, which results in extended decitabine exposure.
“Rapid metabolization, elimination shortens the in vivo exposure and may limit the efficacy of decitabine,” Dr Daver noted. “Guadecitabine was engineered to improve the in vivo levels . . . and the efficacy of decitabine by blocking the rapid elimination.”
In the phase 2 trial, Dr Daver and his colleagues investigated guadecitabine in 103 patients with relapsed/refractory AML. The patients’ median age was 60 (range, 22-82), and 60% were male. Eighty-six percent of patients had an ECOG performance status of 0-1, and 41% had poor-risk cytogenetics.
The median number of prior therapies was 2 (range, 1-7). All patients had received prior chemotherapy, 85% had received prior induction with 7+3 (a continuous infusion of cytarabine for 7 days plus daunorubicin for 3 days), and 18% had a prior hematopoietic stem cell transplant (HSCT).
Fifty-three percent of patients had a CR to first induction, and 47% were primary refractory.
Treatment
The researchers tested 2 different doses and schedules of guadecitabine. In the first cohort (5-day regimen), 50 patients were randomized (1:1) to either 60 mg/m2/day (n=24) or 90 mg/m2/day (n=26) on days 1-5.
In the second cohort (10-day regimen), 53 patients were assigned to treatment with 60 mg/m2/day on days 1-5 and days 8-12 for up to 4 cycles, followed by 60 mg/m2/day on days 1-5 in subsequent cycles.
Cycles were scheduled every 28 days for both regimens. Dose reductions and delays were allowed based on response and tolerability. And patients remained on treatment as long as they continued to benefit without unacceptable toxicity.
Response
The study’s primary endpoint was the CRc rate, which consisted of CR plus CR with incomplete platelet recovery (CRp) plus CR with incomplete neutrophil recovery (CRi).
The CRc rate was 16% in the 5-day cohort and 30% in the 10-day cohort. The CR rate was 6% and 19%, respectively. The CRp rate was 2% and 7%, respectively. And the CRi rate was 8% and 4%, respectively.
There was a trend toward a higher CR/CRc rate with the 10-day regimen (P=0.074 and 0.106, respectively).
There was no significant difference in CRc according to patient age (65 and older vs younger than 65), cytogenetics, prior HSCT, response to induction, or time from last therapy (less than 6 months vs 6 months or more).
However, the CRc rate was significantly lower for patients with an ECOG performance status of 2 than for those with a status of 0-1 (P<0.001).
Survival
For the entire study cohort, the median overall survival (OS) was 6.6 months, the 1-year OS was 28%, and the 2-year OS was 19%.
The median OS was 7.1 months with the 10-day regimen and 5.7 months with the 5-day regimen. This difference was not significant (P=0.51).
The median OS was not reached for patients who achieved a CR or for those who achieved a CRp plus a CRi. For patients who did not achieve a CRc, the median OS was 5.6 months (P<0.01).
The median OS was not reached for patients who had a CRc, whether or not they received a subsequent HSCT. There was no significant difference between patients who received an HSCT post-guadecitabine and those who did not (P=0.87).
Likewise, there was no significant difference in OS according to patient age, prior HSCT, or response to induction.
However, OS was significantly worse for patients with an ECOG performance status of 2 (P<0.001), those with poor-risk cytogenetics (P<0.001), and those for whom 6 months or more had elapsed since their last therapy (P=0.015).
Safety
Common grade 3 or higher adverse events (regardless of the relationship to therapy) were febrile neutropenia (60%), pneumonia (36%), thrombocytopenia (36%), anemia (31%), neutropenia (19%), and sepsis (16%).
The 30-day mortality rate was 3.9%, and the 60-day mortality rate was 11.7%.


