The rate at which medical boards discipline physicians varies widely by state, with Delaware doctors facing four times more disciplinary actions that Massachusetts physicians, according to a review of physicians in all 50 states.
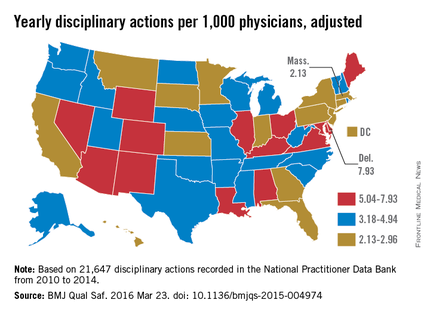
Dr. John Alexander Harris of the University of Michigan, Ann Arbor, and colleagues reviewed 21,647 physician disciplinary actions recorded in the National Practitioner Data Bank from 2010 to 2014 across all 50 states and the District of Columbia (BMJ Qual Saf. 2016 Mar 23; doi: 10.1136/bmjqs-2015-004974).
Investigators evaluated American Medical Association demographic data from the same time frame to estimate rates of disciplinary actions while controlling for the number of physicians in each state. Of the actions studied, 24% were major disciplinary actions involving revocation, suspension, or license surrender. Researchers also controlled for data reliability, year to year variation, physician labor supply, and malpractice climate in each state.
Delaware experienced the highest rate of medical board discipline with eight actions per 1,000 physicians, while Massachusetts had the lowest rate with two actions per 1,000 physicians, the investigators found. Kentucky and Ohio were among the states with the highest rates of disciplinary actions. New York, Connecticut, and Pennsylvania doctors experienced among the lowest rates of medical board disciplinary actions.
Researchers presumed there would be differences in the level of medical board disciplinary actions, but they were surprised at the fourfold gap between states, Dr. Harris said in an interview.
“The biggest takeaway is that there is a large, unexplained variation between the rate at which medical boards discipline physicians from state to state,” he said. “We should focus more on understanding what’s causing this variation.”
Investigators found no significant connection between state medical malpractice climate and the rate of medical board disciplinary actions. They also found no marked association between the rate of disciplinary actions and physician supply or the year of the discipline. No correlation was found between the rate of major and minor disciplinary action. In other words, states that had higher rates of major actions did not necessarily have higher rates of minor actions.
Potential reasons behind the state differences could include variations in the volume of physician misconduct per state, differences in the reporting of misconduct, or disparities in how often medical boards investigate incidents, Dr. Harris said.
“The process of physician disciplinary actions is complex,” he noted. “There are several different steps where the system can change the outcome significantly.”
For more than one-third of actions studied, the basis for the disciplinary action was classified as “unspecified” (38%). Specified reasons included negligence (9%), illegal activity (8%), license action (7%), failure to comply with medical board (6%), fraud (6%), unprofessional conduct (4%), substance abuse (4%), sexual or boundary misconduct (2%), failure to maintain adequate records (2%), immediate threat to public health and safety (1%), and “other” (14%). A total of 5,242 actions had no information regarding the reason for the action.
State medical boards should consider policies aimed at “improving standardization and coordination to provide consistent supervision to physicians and ensure public safety,” the authors wrote. In the meantime, more research is needed in the area, Dr. Harris said.
On Twitter @legal_med