A new low-cost rotavirus gastroenteritis vaccine that does not require cold storage showed a vaccine efficacy of 67% in a per-protocol test of 3,508 Nigerien infants, according to a study by Sheila Isanaka of the department of research at Epicentre, Paris, and her associates.
In a double blind, placebo-controlled test of the oral bovine rotavirus pentavalent vaccine (BRV-PV), 31 severe cases of rotavirus were found in the vaccinated group of 1,780, while 87 cases were found in the placebo group of 1,728 (2.14 vs. 6.44 cases per 100 person-years, respectively), according to Ms. Isanaka and her colleagues (N Engl J Med. 2017 Mar 23;376[12]:1121-30).
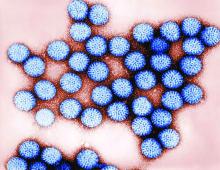
Researchers gathered infants with severe symptoms and administered three injections of either BRV-PV or the placebo from August 2014 through November 2015. The BRV-PV vaccine, manufactured by Serum Institute of India, contains the rotavirus serotypes G1, G2, G3, G4, and G9.
With regard to adverse events, there was no distinction between the two groups (P greater than .15). According to medical investigators, the most common cause of deaths – 27 and 22 in the vaccine and placebo groups, respectively – was infections and infestations (in 37 infants) and metabolism and nutrition disorders (in 6).
Part of what makes this vaccine unique is its shelf life of 2 years when kept at 37° C, or 6 months at 40° C, a key point for Ms. Isanaka and her colleagues.
“The global supply of the vaccines is constrained, and unreliable transportation and storage systems make delivery of vaccines that require refrigeration difficult,” Ms. Isanaka and her colleagues reported. “The introduction of BRV-PV may help to minimize the burden on already strained immunization programs.” The vaccine is also “for sale at or below the current price of the two WHO prequalified vaccines that are supported by the Gavi alliance,” making it possibly more financially accessible as well.
While the per-protocol test found efficacy at 67%, the intention-to-treat population reported a higher efficacy of 73%. Ms. Isanaka and her colleagues believe this number “may more closely represent the efficacy under real-world conditions,” due to the more flexible vaccination schedule.
This study was limited by a short time frame, which did not allow researchers to gather genotyping data pertaining to the efficacy against changing serotypes. BRV-PV also was not given consistently with the oral polio vaccine.
The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets