In treating the emerging virus MERS-CoV, two antivirals already licensed to treat hepatitis C should be considered for early intervention therapy, according to researchers from the National Institute of Allergy and Infectious Diseases.
This research, based upon favorable results in a rhesus monkey model of Middle East respiratory syndrome coronavirus (MERS-CoV), comes at a time of great interest in the progression of the MERS-CoV outbreak, currently restricted to the Middle East. As of this writing, the World Health Organization reported that from September 2012 to date, WHO had been informed of a total of 114 laboratory-confirmed cases of infection with MERS-CoV with 54 deaths, including those of health care workers involved in treating infected individuals.
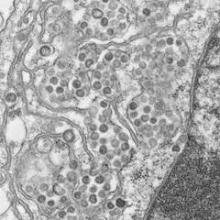
Dr. Darryl Falzarano and his colleagues at the National Institutes of Health’s (NIH’s) National Institute of Allergy and Infectious Diseases (NIAID) demonstrated that a combination of ribaravin and interferon alpha-2b stopped MERS-CoV replication in cell culture and improved clinical outcomes in infected monkeys, using a model system for the disease reported on earlier this year in the New England Journal of Medicine (2013;368:1560-2).
In a Sept. 8 release, the NIH announced publication of a letter in Nature Medicine detailing how treatment of rhesus macaques with the two antivirals 8 hours after inoculation with MERS-CoV affected the progression of disease as compared to untreated controls. Treated animals did not develop breathing abnormalities and had "no or very mild radiographic evidence of pneumonia. Moreover, treated animals showed lower levels of systemic (serum) and local (lung) proinflammatory markers, in addition to fewer viral genome copies, distinct gene expression, and less severe histopathological changes in the lungs," according to the researchers (Nat. Med. 2013 Sept. 8 [doi: 10.1038/nm.3362]).
The proposed intervention is similar to that found effective for the earlier, similarly behaving SARS (severe acute respiratory syndrome) virus. "The clinical experience from SARS suggests that a number of interventions, including ribavirin with and without corticosteroids, interferon-alfa with corticosteroids, ribavirin with lopinavir and ritonavir, and convalescent plasma may improve the outcome in patients but the data are not conclusive," wrote Dr. Hisham Momattin and his colleagues, who assessed therapeutic options for MERS-CoV in a systematic review of SARS therapy appearing in the International Journal of Infectious Diseases (2013;17:e792-e798).
"The high case fatality rate [currently seen] is likely related to the pattern of the disease, as we probably are seeing only the tip of the iceberg of critically ill and admitted patients. The high fatality rate is likely to decline as milder clinical cases emerge. Similar to SARS, common symptoms in patients with MERS-CoV include fever, cough, shortness of breath, and gastrointestinal symptoms. Most patients have had pneumonia, and the majority was reported to have multiple comorbid conditions," Dr. Momattin and his colleagues said. "The rapid deployment of effective therapeutics is a high priority, as there is currently no specific therapy or vaccine for MERS-CoV," they added.
Because the virus has been seen to be transmitted to and even kill health care workers in close contact with infected individuals, most authorities are recommending precautions in the treatment of patients suspected to have MERS-CoV.
In a recent overview, Dr. Jaffar Al-Tawfiq pointed out that the exact mode of transmission of the virus is not yet known, and addressed the advised containment protocol for hospital health care workers: "When caring for patients with suspected or confirmed cases of MERS-CoV, the following recommendations for infection control measures in hospital settings include: standard precautions; droplet precautions (wearing a medical mask when in close contact (within 1 m) and upon entering the room or cubicle of the patient); and performing hand hygiene in accordance with the World Health Organization’s (WHO’s) five moments of hand hygiene. Additional measures include wearing a particulate respirator when performing aerosol-generating procedures in addition to other precautions as outlined by WHO," (J. Infect. Public Health 2013;6:319-22).
Dr. Al-Tawfiq discussed a MERS-CoV outbreak in a health care setting where there was evidence of person-to-person transmission, and the outbreak was aborted by the implementation of basic infection control measures. He pointed out that the Centers for Disease Control and Prevention in the United States recommended placing the patient in an airborne-infection isolation room.
For those questioning the relevance of such dedicated research and investment of resources in narrowly focused emergent diseases, Dr. Hanan Balkhy, editor in chief of the Journal of Infection and Public Health, had an answer in her recent editorial (J. Infect. Public Health 2013;6:317-18). "Today the current viruses, whether the novel MERS-CoV or any of the emerging influenza viruses, do have the potential capacity to evolve into acquiring the ability to sustained human-to-human transmission. And therefore, we will continue to hope for the best and act as if it is the worst. In doing so, the infectious disease community will be criticized for being overstated in their policies and take the heat as they have in the past with similar scenarios, such as the H1N1 pandemic. I just hope people realize that hindsight is always 20/20."