SAN FRANCISCO – Four critical care societies released a list of the top five things that intensivists should avoid doing, part of the larger Choosing Wisely campaign to reduce unnecessary and costly medical practices. The list includes a potentially difficult issue: offering patients' families the option of comfort care in lieu of continuing life support.
Fifth on the list, the life-support item may be the most controversial and is also the one that the representatives felt the most strongly about including, whether or not it saves many resources, according to Dr. Hannah Wunsch, who served on the collaborative task force. "Many ... patients receive aggressive life-sustaining therapies, in part due to clinicians’ failures to elicit patients’ values and goals, and to provide patient-centered recommendations," the task force wrote.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel.
Discussion of the list, which was announced at the Critical Care Congress, quickly turned to how to implement the recommendations, including how to empower families to challenge physicians or nurses when they see these steps being taken in the care of a loved one.
The Society for Critical Care Medicine, which sponsored the Congress, collaborated with the American College of Chest Physicians, the American Thoracic Society, and the American Association of Critical Care Nurses to create the list. It’s the first Choosing Wisely list to include collaboration with a nursing organization and only the second that’s a product of collaboration instead of being issued by a sole medical society, said Dr. Scott D. Halpern of the University of Pennsylvania, Philadelphia, chair of the collaborative group.
The four groups – the Critical Care Societies Collaborative – started with a list of 58 medical practices that they found objectionable, which they trimmed to 9 items based on the strength of evidence and their prevalence, relevance, and cost, explained Dr. Wunsch of the department of anesthesiology at Columbia University Medical Center, N.Y. Discussion winnowed that to the Top 5, an arbitrary number selected by the Choosing Wisely campaign that everyone should recognize as "a starting point," she said.
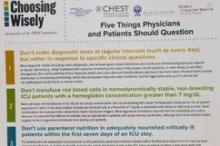
A two-page document of the critical care list can be downloaded from the Choosing Wisely website. It includes some of the sources for the recommendations and these top five "don’ts" displayed on the front:
1. Don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions. Ordering diagnostic studies such as x-rays, arterial blood gases, blood counts, blood chemistries, or ECGs daily or at routine intervals drives up costs, doesn’t benefit patients, and may harm them through radiation exposure, inducing anemia, or triggering aggressive follow-up of incidental results. "I think this has become more prevalent with electronic medical records," where one click can order x-rays for the next 5 days, she said.
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 mg/dL. Blood is a scarce resource, and studies show that limiting red blood cell transfusions to thresholds of 7 mg/dL or higher does not worsen survival, complications, or costs, and causes fewer complications. Different thresholds may be appropriate for patients with acute coronary syndrome, but even in this subgroup aggressive transfusion is harmful, most observational studies suggest.
3. Don’t use parenteral nutrition in adequately nourished critically ill patients within the first 7 days of an ICU stay. Early parenteral nutrition is harmful, even in patients who cannot tolerate enteral nutrition, if they were adequately nourished prior to ICU admission. The evidence is less clear for patients with nosocomial infections, and early parenteral nutrition may benefit patients who were severely malnourished right before ICU admission.
A study to be published soon shows that 90% of parenteral nutrition in the United States starts within 7 days of admission, usually within the first 2 days, Dr. Wunsch said. "It’s definitely more prevalent than I think many of us realize," she said.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Deep sedation of patients on mechanical ventilation prolongs the duration of ventilation and hospitalization. Several protocols for limiting sedation have been shown to improve patient outcomes.
5. Don’t continue life support for patients at high risk of death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. When an audience member expressed concern about discontinuation of life support possibly increasing premature deaths, Dr. Wunsch stressed that the second part of the statement is key – giving the family the choice of comfort care or continuing life support.