Video

Webcast: Obesity and contraceptive efficacy and risks
What you should know before counseling your obese patients on choosing a contraceptive

Dr. Barbieri is Editor in Chief, OBG Management; Chair, Obstetrics and Gynecology, Brigham and Women’s Hospital; and Kate Macy Ladd Professor of Obstetrics, Gynecology, and Reproductive Biology, Harvard Medical School, Boston, Massachusetts.
Dr. Barbieri reports no financial relationships relevant to this article.

There’s a nationwide gap in contraceptive services—many reproductive-aged women with serious medical problems are not receiving adequate contraception
In the United States contraception practices are slowly improving, with robust evidence for the increased use of long-acting reversible contraceptives and preliminary data that the unintended pregnancy rate may be decreasing for the first time in many years.1 There remains a major gap in contraception practice, however: US women with chronic disease who are at high risk for adverse pregnancy outcomes are not receiving adequate contraceptive counseling or adequate contraception.2,3 In one study, the majority of women with hypertension, diabetes, epilepsy, stroke, heart disease, lupus, or thrombophilia were not using a prescription contraceptive.3
Recently, I have seen women with major medical problems, who have had many visits with specialists and primary care clinicians, but who have not had their contraceptive needs prioritized. Here are but a few examples:
Clearly, there is a major gap between current and optimal contraceptive services for women with chronic medical problems. Women with diabetes and heart disease are affected substantially, as the evidence I present in this editorial indicates. Studies also show that women taking teratogenic medications do not receive the vital counseling that they should regarding contraception. Given the potential detrimental adverse events to both mother and fetus, obstetrician-gynecologists are poised to offer solutions to this concerning inadequacy of care.
DiabetesWomen with diabetes and an abnormally elevated HbA1c level are at high risk for many adverse pregnancy outcomes, including major congenital malformations and intrauterine fetal demise.4 Unfortunately, results of many studies indicate that women with diabetes are not receiving adequate contraceptive services.5–7 In one review of records at Kaiser Permanente Northern California, investigators reported that 62% of 122,921 healthy women, but only 48% of 8,182 women with diabetes, received contraceptive counseling, a contraceptive prescription, or contraceptive services.5
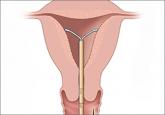
Why is it that so many women with diabetes do not receive contraceptive services? One possibility is that clinicians are reluctant to prescribe oral hormonal contraceptives that contain estrogen to their patients with diabetes because of a perceived increased risk of cardiovascular events.8 In the Kaiser study, 31% of the healthy women, and only 13% of the women with diabetes, were using a pill, patch, or ring (most of which contain estrogen).5 In this same study, the rate of utilization of an IUD was similar in the healthy (6.5%) and diabetic (5.6%) women. The IUD is known to be safe for use in women with diabetes.9
The low rate of utilization of intrauterine contraception by women with diabetes is a gap that gynecologists are well positioned to help solve.
Heart diseaseIn developed countries, a major cause of maternal mortality is pregnancy among women with congenital or acquired heart disease.10 Misinformation is a common problem in contraceptive counseling. In a recent study of 83 sexually active women with congenital heart disease, 6 women were told that they could not use an IUD or progestin-implant because they were unsafe for those with repaired congenital heart disease.11 In this cohort of women, who were at high risk for adverse pregnancy outcomes, 45% of pregnancies were unplanned, similar to the rate among healthy women.
On a positive note, authors of a small study from Maryland found that, among women with heart disease, the self-reported use of a contraceptive increased from 60% prepregnancy to 93% following delivery.12
Clearly, patient interaction with qualified women’s health clinicians can increase contraceptive use in those with high-risk medical issues.
Teratogenic medicationsShould reproductive-age women taking long-term methotrexate for treatment of rheumatoid conditions receive contraceptive counseling? The answer is clearly, “yes.” Methotrexate can cause fetal death or major congenital malformations, such as absence of digits and oxycephaly (premature closure of the skull sutures). All women of reproductive age prescribed known teratogens should receive effective contraception. Unfortunately, data do not indicate this is occurring.
In one study of 1,694 adolescents and young women aged 14 to 25 years who were prescribed a teratogen, only 29% received documented contraception counseling, and only 11% received a contraceptive prescription or were documented to be actively using a contraceptive.13 The most commonly prescribed teratogens in this study were topiramate, methotrexate, and isoretinoin. Among the specialists who prescribed the medications, dermatologists documented contraceptive counseling in 47% of visits—likely because of the federally mandated risk mitigation system for prescribing isoretinoin. Neurologists and hematologists were least likely to document contraceptive counseling, at 16% and 28%, respectively.13

What you should know before counseling your obese patients on choosing a contraceptive

Mastering these resources for contraception and condition compatibility could go a long way during busy days of patient care
Although use of long-acting reversible contraception is increasing slowly in the United States, there is plenty of room for improvement,...

The US unintended pregnancy rate has reached an all-time high. Two experts explore the roots of the problem (cost most paramount) and offer...
The unintended pregnancy rate is too high in the United States, and the use of long-acting reversible contraceptives is too low. Expanding the...
