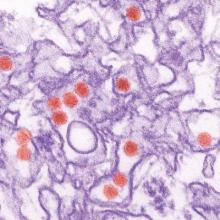
The link between Zika virus infections in pregnant women and microcephaly in neonates is strong, and there is good if somewhat less robust evidence for the virus causing severe neurological sequelae, especially Guillain-Barré syndrome, world health experts say.
Zika virus outbreaks have been reported in 31 countries and territories in the Americas, totaling more than 135,000 reported cases, and about 3,000 laboratory-confirmed cases, Dr. Marcos Espinal, director of the department of communicable diseases and health analysis at the Pan American Health Organization/World Health Organization, said at a joint PAHO/WHO meeting announcing key findings from an international meeting on the global challenge from Zika virus.
“The reports of these cases do not reflect the real situation, as in 80% of the cases globally there have been no signs and symptoms of Zika disease,” Dr. Espinal said.
Although the epidemic has garnered worldwide attention, there are many more unknowns than knowns about Zika virus and its sequelae, and recent findings from the outbreak are of particular concern, noted Dr. Lyle Petersen of the Centers for Disease Control and Prevention in Atlanta.
“It’s the first vector-borne disease we’ve seen that’s caused infections in fetuses and abnormal birth outcomes, and it’s also the first vector-borne disease that is also readily spread via sexual means,” he said.
To date, cases of microcephaly in the fetuses of Zika-infected women have been reported only in Brazil and in French Polynesia. As of Feb. 23, 2016, 5,640 cases of microcephaly had been reported in Brazil. In French Polynesia, as reported in The Lancet, following an epidemic of Zika from September 2013 through March 2014 affecting an estimated 28,000 individuals (about 11.5% of the population), clinicians noted an increase in cerebral congenital abnormalities, including microcephaly, ventriculomegaly, severe abnormalities of midline structures and the cerebellum, and abnormal gyration.
In addition, an increase in the incidence of Guillain-Barré syndrome cases coinciding with Zika virus outbreaks has been reported in Brazil, Colombia, El Salvador, Suriname, and Venezuela.
Resistant mosquitoes
Dr. Paulo Buss, director of the Global Health Center at the Oswaldo Cruz Foundation in Brazil, acknowledged that his country was the epicenter of the current epidemic, but noted that Brazil’s surveillance system was quick to identify the onset of the epidemic and make connections between Zika infection and its affect on congenital malformations and neurological disease. He pointed out that the epidemic is taking an especially hard toll on Brazilians with low incomes, who often live in overcrowded, unsanitary conditions, with no running water and no window screens to protect against mosquitoes.
One of the greatest challenges to public health authorities is the hardiness and adaptability of the vector, the Aedes aegypti and Aedes albopictus mosquitoes that are also prime vectors for dengue, chikungunya, and yellow fever infections, Dr. Buss said.
That point was reinforced in a recent report in The Lancet by Brazilian researchers who said that although their government has recently intensified efforts to eliminate Aedes aegypti using insecticides to kill adult mosquitoes and larvicides to eradicate breeding pools, “the results have been very disappointing.”
Despite mosquito eradication efforts, there has been an increase in the incidence of registered dengue cases in Brazil, with 1.6 million cases and 863 deaths reported in 2015. In addition, growing resistance by the vector to pesticides has forced health authorities to try a succession of different agents, further increasing the likelihood of resistance.
Areas of need
World health authorities broadly agreed, Dr. Espinal said, on the need for improved laboratory detection of infections, particularly a rapid and accurate test for pregnant women. Research questions must focus on both clinical research into prevention and treatment of infection, but also public health issues such as more effective vector control.
“This is a unique situation,” said the CDC’s Dr. Petersen. “I’ve been studying vector-borne diseases spread by mosquitoes for more than 20 years, and I’ve never seen anything like this.”
The situation calls for a research-guided response, he said, with collaboration and support from government and nongovernment organizations, WHO, PAHO, and academic institutions. The response must also be very rapid, as thousands of new infections are occurring in the Americas daily, he added.
“I think this outbreak reminds us that we all must be prepared. Over the last decade, we have let our responsibilities for vector-borne disease deteriorate. Mosquito control programs have gone away, and we’ve not developed any new pesticides in 50 years,” Petersen said. “This is a very good reminder that new things happen, and unexpected things happen, and we must be prepared.”