WASHINGTON – An investigational drug for sickle cell disease (SCD) boosted hemoglobin levels while reducing hospitalizations and transfusion needs by approximately two-thirds in a small cohort of severely affected patients.
Seven patients received the new, once-daily oral medication – voxelotor – under the Food and Drug Administration’s expanded access, or compassionate use, exemption.Lanetta Bronté, MD, who presented the findings at the annual meeting of the Foundation for Sickle Cell Disease Research, reviewed the FDA’s requirements for allowing expanded access to an investigational drug. The key point, she said, is that expanded access may be granted “for treatment of patients with serious or immediately life-threatening diseases or conditions that lack therapeutic alternatives.” And, she said, the potential for benefit should outweigh potential risk of taking the investigational drug.
Current treatments don’t really address serious disease-related complications for patients with advanced SCD, she said. Furthermore, these patients will often be excluded from clinical trials of new SCD therapies.
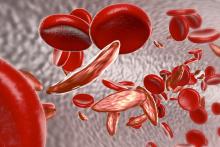
Voxelotor is a novel small molecule that stabilizes the sickle hemoglobin molecule as a monomer in its high oxygen state. Thus, polymerization of the hemoglobin molecules is inhibited, which decreases the amount of red blood cell damage. Other beneficial effects of voxelotor include improved rheology and reduced hemolysis, as well as a boost to the oxygen-carrying capacity of the sickle hemoglobin molecules, Dr. Bronté explained.
For the seven patients in Dr. Bronté’s clinic who were granted expanded access to voxelator, the disease burden of their end-stage SCD was heavy. All participants had iron overload, five were receiving frequent transfusions, two required chronic oxygen supplementation, and four had severe fatigue. One patient had end-stage renal disease, and another had experienced multiple organ failure and prolonged hospitalizations.
None of the patients qualified for participation in ongoing clinical trials of voxelotor, said Dr. Bronté, who is president of the Foundation for Sickle Cell Disease Research. She also maintains a private practice in Hollywood, Fla.
The four women and three men, aged 22-67 years, were treated with voxelotor for a range of 6-17 months under the FDA’s Expanded Access Program. All patients saw rapid increases in serum hemoglobin, with increases of at least 1 g/dL in five of the seven. Across the participants, increases ranged from 0.5-5.4 g/dL at 24 weeks, up from baseline values of 5.2-7.8 g/dL.
One marker of clinical efficacy that Dr. Bronté and her coauthors examined was the number of hospitalizations for pain from vaso-occlusive crises (VOCs). In the 24 weeks before beginning voxelotor, participants had a summed total of 28 hospitalizations. In the first 24 weeks of treatment, there were a total of nine VOC-related hospitalizations among the participants, a 67% decrease.
The total number of red blood cell transfusions required by the study population declined by a similar proportion, from 33 during the 24 weeks before voxelotor treatment to 13 during the first 24 weeks of treatment, a decrease of 60%.
Individual patients saw improvements related to some of their most troublesome SCD complications, Dr. Bronté reported. All four patients whose oxygen saturation levels had been below 95% on room air saw oxygen saturations improve to 98%-99% on voxelotor. The two patients who had moderate or moderately severe depression, as assessed by the Patient Health Questionnaire 9-item, had minimal or no depression on retest after 24 weeks of voxelotor treatment.