CASE Embedded IUD, currently asymptomatic patient
A 32-year-old G4, P3 presents 1 day after pelvic ultrasonography (US) is performed to evaluate a previous report of intermittent left lower quadrant pain. She is using a levonorgestrel-intrauterine system (LNG-IUS) for contraception, which was placed 1 year ago when she was 6-weeks postpartum. She previously had heavy menses but now has minimal bleeding and is happy with her intrauterine device (IUD). US showed that the IUD is in the lower uterine segment, with the left arm embedded in the myometrium (FIGURE 1). The patient’s pain resolved spontaneously 2 weeks ago, and she is now asymptomatic.
What were this patient’s risk factors for IUD malpositioning? How would you manage her at this time?
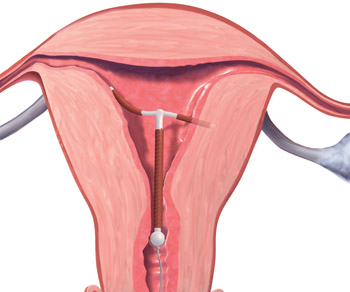
FIGURE 1 Copper intrauterine device displaced in the lower uterine segment with the left arm embedded in the myometrium.IUDs are an increasingly common form of birth control, now used by 5.5% of contracepting women in the United States.1 With frequent use of pelvic US to evaluate gynecologic complaints, the discovery of malpositioned IUDs also has become an increasingly common occurrence. Clinicians often find themselves faced with dilemmas regarding how to manage a malpositioned IUD, especially in the setting of an asymptomatic patient.
In this article, we review: 1) what constitutes a malpositioned IUD, 2) the consequences of malpositioning, 3) how or if malpositioning can be avoided, and 4) how to manage a malpositioned IUD.
Let’s increase our use of IUDs and improve contraceptive effectiveness in this country
Robert L. Barbieri, MD (Editorial, August 2012)
Update on Contraception
Tami Rowen, MD, MS; Mitchell D. Creinin, MD (August 2012)
What constitutes malpositioning?
A correctly positioned IUD should be located at the fundus of the uterus, with the arms fully expanded and extending toward the uterine cornua. The vertical portion of the “T” should extend straight down in the uterine corpus. When noted on US, malpositioned IUDs may be described as:
- located in the lower uterine segment or cervix
- rotated (FIGURE 2)
- embedded in the myometrium (one or both arms) (FIGURE 3)
- partially expelled (if an IUD is low enough in the cervix that the hub extends through the external os), or
- protruding through the uterine serosa or completely outside the uterus and within the abdominal cavity. (This is how a perforated or partially perforated IUD may be described.)
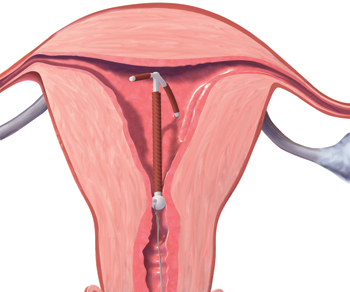
FIGURE 2 Rotated IUD
Copper intrauterine device rotated horizontally.
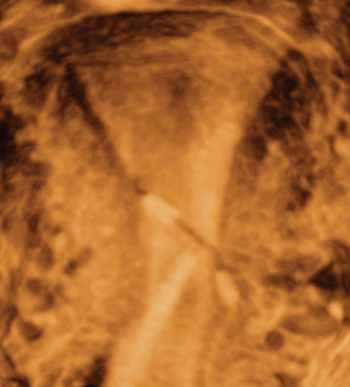
FIGURE 3 Embedded IUD
Three-dimensional sonogram of a 26-year-old patient, showing an intrauterine device displaced in the lower uterine segment with the left arm embedded in the myometrium.If US does not show an IUD that has been placed, x-ray should performed to explore for perforation (see algorithm.)
What damage can malpositioning cause?
For many women, a malpositioned IUD may have minimal or no adverse consequences. The most common negative sequelae of women with a malpositioned IUD, however, include an increase in bleeding or pain, compared with women with fundally positioned IUDs.
Bernacerraf and colleagues retrospectively reviewed the medical records of 167 consecutive women who had ultrasound examination with an IUD in place and found that 28 (16.8%) of them had malpositioned devices.2 Of these 28 women, 75% presented with either bleeding or pain, compared with 34.5% of women with normally positioned devices (P=.0001). Twenty of the 21 patients with a malpositioned device and symptoms reported improvement in their symptoms after IUD removal. In this study, the type of IUD was not specified.
Similar to Bernacerraf and colleagues, authors of a case-controlled study, in which women with malpositioned IUDs were compared with women with normally positioned IUDs, found a higher proportion of symptoms, including bleeding and pain, among women with malpositioned IUDs.3 This study included both copper and levonorgestrel IUDs.
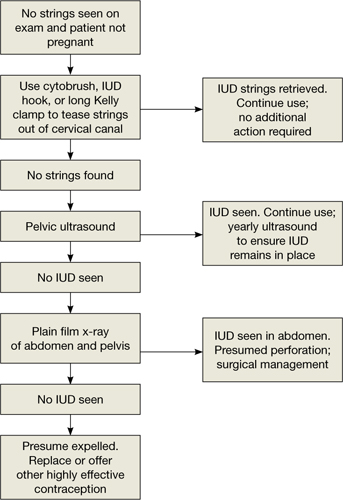
The bowel can suffer, though on rare occasion. The rarest, though most serious form of IUD malpositioning, is the IUD that has perforated the uterine corpus and is intraperitoneally located (FIGURE 4). Studies suggest that approximately 15% of these perforated IUDs cause injury or damage to surrounding organs, primarily the bowel. Management of intraperitoneal IUDs generally involves laparoscopy or laparotomy for removal and exploration of the surrounding structures.4
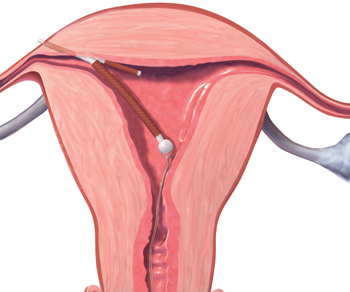
FIGURE 4 Perforation
A copper intrauterine device perforating the serosa.
What about risk of pregnancy?
For the asymptomatic patient, your biggest concern often is whether a malpositioned IUD poses an increased risk of pregnancy. Though data are limited, the available literature suggests that malpositioned, specifically cervically located, copper IUDs may pose an increased risk of pregnancy.
In a prospective study, the authors compared 97 women who had a Cu375 Multiload IUD inserted with 25 women in whom pregnancy was discovered with an IUD in place.5 They found a greater occurrence of intracervical IUDs among the pregnant women, with an odds ratio of 13.93 for pregnancy among women with cervically versus correctly positioned IUDs. Similarly, findings from a case-control study, in which 318 women with pregnancies with CuT380A IUDs in place were compared with 300 controls also using the CuT380A IUD, revealed a 64% rate of IUD malpositioning among the pregnant cases, compared with an 11% rate among the nonpregnant controls (P<.05).6

