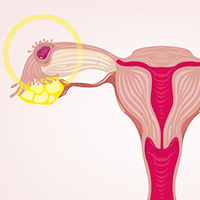
Ectopic pregnancy misdiagnosed
When a patient called her ObGyn (Dr. A) to report that she was 6 weeks' pregnant and had lower abdominal pain, she was seen by his partner (Dr. B). Dr. B could not identify an intrauterine pregnancy using ultrasonography (US), but the patient's hCG level was highly suggestive of an ectopic pregnancy. The next day, Dr. B performed exploratory laparoscopy, found no evidence of an ectopic pregnancy, and removed the patient's appendix. He continued to be concerned about the possibility of an ectopic pregnancy and suggested that the patient terminate the pregnancy. The next day he prescribed methotrexate. A week later, US revealed a fetus in utero with a beating heart. Because of the likelihood of birth defects after methotrexate use, Dr. B recommended terminating the pregnancy; an abortion was performed a month later.
PATIENT’S CLAIM:
Dr. B should have waited for the pathology report on the appendix and repeated the US before rushing into advising termination of pregnancy.
PHYSICIAN’S CLAIM :
Dr. B acted reasonably based on the patient's symptoms.
VERDICT:
A Kentucky defense verdict was returned.
Related article:
Stop using the hCG discriminatory zone of 1,500 to 2,000 mIU/mL to guide intervention during early pregnancy
Hemorrhage after trocar insertion
A gynecologist performed laparoscopic hysterectomy on his 46-year-old patient. During trocar insertion, the patient's iliac artery, iliac vein, and small bowel were injured. The patient hemorrhaged and went into cardiac arrest. The patient was given several transfusions and the injuries were repaired.
One day after discharge, she returned to the hospital with symptoms of an embolism; she was treated with anticoagulants for 1 year. A year after surgery, she was informed that she was transfused during surgery with HIV-positive blood. Her initial HIV test came back negative.
PATIENT’S CLAIM:
The gynecologist deviated from the standard of care by performing a "blind" trocar insertion, which caused the major vessels to be more susceptible to injury.
PHYSICIAN’S DEFENSE:
There was no deviation from the standard of care. Blind insertion of a trocar is an acceptable procedure.
VERDICT:
A $383,000 Illinois verdict was returned.
Related article:
How to avoid major vessel injury during gynecologic laparoscopy
Delay in ovarian cancer diagnosis: $1.9M settlement
A 64-year-old woman reported worsening abdominal pain, fatigue, and unexplained weight loss to her primary care physician. The physician did not order tests to assess the patient's status; he diagnosed gastritis. Several months later the patient saw another physician, who ordered imaging and identified stage IV ovarian clear cell carcinoma.
PATIENT’S CLAIM:
Timely imaging would have diagnosed ovarian cancer at stage I or II and given her a 90% survival rate at 10 years. Due to the diagnostic delay, her survival rate was less than 10% at 10 years.
PHYSICIAN’S DEFENSE:
The case settled before trial.
VERDICT:
A $1.9 million Illinois settlement was reached.
Late breast cancer diagnosis: $1.7M settlement
When a 25-year-old woman found a lump in her left breast she saw her gynecologist, who recommended US and fine-needle aspiration biopsy. US results indicated possible cancer; biopsy results were reported as negative for cancer. No further action was taken.
Eight months later, a second physician diagnosed stage IV breast cancer requiring chemotherapy, radiation therapy, and multiple surgeries.
PATIENT’S CLAIM:
The radiologist misread the fine-needle aspiration biopsy results. The gynecologist should have ordered a core needle biopsy because it is more reliable.
PHYSICIAN’S DEFENSE:
The case was settled during the trial.
VERDICT:
A $3.5 million Illinois settlement was reached.
Perforated colon after oophorectomy
A 55-year-old woman underwent laparoscopic oophorectomy to address pelvic pain and a right ovarian mass. Following surgery she developed peritonitis and sepsis. She underwent a colon resection with colostomy and had severe keloid scarring.
PATIENT’S CLAIM:
The surgeon was well aware of her history of extensive pelvic adhesions. Given her medical history, he should have performed an open laparotomy.
PHYSICIAN’S DEFENSE:
The case settled during trial.
VERDICT:
A $700,000 Illinois settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.

