This approach to testing has a serendipitous advantage: It isn’t associated with a massive increase in cost for additional testing.
Many hurdles ahead
The risk of late fetal loss is influenced by many variables, including:
- gestational length
- maternal age
- race and ethnicity (see the FIGURE )
- parity
- level of education
- history of fetal loss
- numerous maternal and fetal diseases (e.g., maternal diabetes, hyperthyroidism, and hypertension; fetal growth restriction and congenital anomalies).
Key word: “Optimize.” The question of how to develop clinical algorithms that optimize pregnancy outcome by identifying an optimal upper limit of an optimal time for delivery hasn’t been answered because the matter hasn’t been exhaustively studied in randomized trials. It will be a challenge to validate such algorithms, because any strategy runs the risk of utilizing substantial health-care resources for modest clinical gain.3–5
Until sophisticated, multifactorial algorithms for identifying an optimal due date are developed, clinicians are left to select a few prominent variables to guide their recommendations—such as gestational length and maternal age. For a healthy woman, expectant management of pregnancy beyond 41 weeks is associated with an increase in the rates of stillbirth; meconium staining and meconium aspiration syndrome; and cesarean delivery. Based on these observations, many obstetricians routinely offer elective delivery to women who have reached 41 weeks’ gestation but have not begun spontaneous labor.6
As I noted, in addition to gestational age, such variables as the mother’s age and race influence optimal timing of delivery. Examples: For a woman 40 to 44 years old, delivery between 38 and 39 weeks’ gestation may be optimal to prevent stillbirth. For a woman 25 to 29 years old, it is likely safe to allow the pregnancy to progress to 41, possibly 42 weeks’ gestation before delivery.7
In addition, given the increased risk of stillbirth among black women ( FIGURE ), it might be reasonable to consider using race to 1) guide the decision to initiate fetal testing and 2) determine the optimal time for delivery.8,9
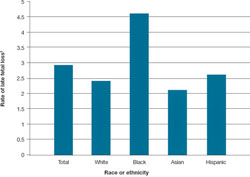
FIGURE Looking by race and ethnicity, blacks have the highest rate of late* fetal loss
*28 weeks or later.
† For every 1,000 (total) births beyond 20 weeks’ gestation.
Adapted from: Centers for Disease Control and Prevention. MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vit Stat Rep. 2009;57:1–20.
4,000 fewer tragedies would be a blessing
With 4 million births annually in the United States, a late fetal loss rate of 3 for every 1,000 total births means 12,000 near-term stillbirths. Monitoring fetal movement, and responding promptly and in a standardized manner when it decreases, would reduce late fetal loss by 33%. That is 4,000 more live births, every year.
Look how a small shift in practice can bring a significant change in outcome—each one of those babies a precious gift to a mother and family!


