Surgical Techniques
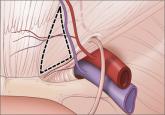
Anatomy for the laparoscopic surgeon
Laparoscopic surgery is a safe and effective option for many patients, provided the surgeon knows the relevant anatomic landmarks and variations...
ESTATE’S CLAIM Both the MFM and the ObGyn failed to recognize placenta accreta on US prior to delivery. The ObGyn should have performed US prior to beginning cesarean delivery. The hospital’s protocols were not followed: the ObGyn should have stopped the procedure and called for extra surgical assistance and additional blood when he encountered placenta accreta, and again when the patient began to hemorrhage. Placenta accreta does not have to be fatal if detected and managed properly.
DEFENDANTS’ DEFENSE There was no negligence; the patient was treated properly.
VERDICT A $15.5 million Illinois verdict was returned against both physicians and the medical center.
Related article: Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence, December 2013)
ANTICONVULSANT AND MIGRAINE MEDS TAKEN DURING PREGNANCY
A woman was prescribed topiramate (Topamax) for migraine headaches and hand tremors during the first trimester of her pregnancy in 2007. With a history of seizures, she also took several anticonvulsants throughout her pregnancy. Her child was diagnosed with right unilateral cleft lip (cheiloschisis) in utero. The condition had not been surgically corrected at the time of trial.
PARENTS’ CLAIM The use of topiramate caused the child’s cleft lip. Janssen Pharmaceuticals, the manufacturer of Topamax, knew about the risk of birth defects associated with the drug in 2007, but failed to provide adequate warnings.
DEFENDANTS’ DEFENSE The mother received at least two warnings from her physician regarding the potential risks of anticonvulsant and antiepileptic drugs and the importance of not becoming pregnant while taking the medications. An action against the physician was barred by the applicable statute of limitations. The mother had taken topiramate prescribed to her mother for a time; such actions should release Janssen from liability.
VERDICT A $11 million Pennsylvania verdict was returned.
PID MASKS ECTOPIC PREGNANCY
A woman in her 40s became pregnant. On the first two prenatal diagnostic imaging studies, the ObGyn saw an intrauterine pregnancy. He later realized that the pregnancy was ectopic after beta human chorionic gonadotrophin (beta-hCG) blood levels were abnormal. During surgery to terminate the pregnancy, he found he had to perform a total hysterectomy because the patient had extensive pelvic inflammatory disease (PID) caused by a long history of sexually transmitted disease.
PATIENT’S CLAIM If the ectopic pregnancy had been diagnosed earlier, one of her ovaries could have been preserved, saving her from the symptoms of surgical menopause.
PHYSICIAN’S DEFENSE PID had caused the ovaries, numerous fibroid tumors, and the uterus to fuse into one mass. That was why the first two imaging studies appeared to show an intrauterine pregnancy. It was not possible to diagnose the extent of the problem until surgery. The patient did not have a true ectopic pregnancy.
The patient’s difficulties occurred during a 2-week time period in which she had one visit with him and another visit to an ED where two other physicians examined her and missed the diagnosis.
VERDICT A Michigan defense verdict was returned.
ILIAC ARTERY INJURED DURING LAPAROSCOPIC SURGERY; PATIENT DIES
A 40-year-old woman underwent laparoscopic gynecologic surgery performed by her ObGyn. During the procedure, the patient’s left internal iliac artery was punctured, but the injury was not recognized at the time. She was discharged the same day. The next morning, she went into hypovolemic shock due to internal bleeding. She was taken to the ED, where she died.
ESTATE’S CLAIM The ObGyn, anesthesiologist, and hospital staff were negligent in their postoperative care. The anesthesiologist prescribed pain medication that masked the injury; the patient was discharged from the postanesthesia unit too early and without proper examination. The nursing staff did not react to the patient’s reports of abdominal pain, nor did they properly assess her condition prior to discharge. The ObGyn failed to return a phone call the evening after the procedure.
DEFENDANTS’ DEFENSE The ObGyn settled before trial. The anesthesiologist and hospital denied negligence: care was proper and followed all protocols.
VERDICT A confidential California settlement was reached with the ObGyn. A defense verdict was returned for the anesthesiologist and hospital.
Related article: Anatomy for the laparoscopic surgeon Emad Mikhail, MD; Lauren Scott, MD; Stuart Hart, MD, MS (April 2014)
GENETIC TESTING MISSED A KEY DIAGNOSIS
A 40-year-old woman underwent genetic testing after she became pregnant. She was assured that there were no abnormalities that would impact her child.
The baby was born with Wolf-Hirschhorn syndrome, characterized by facial deformities, intellectual disabilities, delayed growth, and seizures. The child is nonverbal, deaf, and blind. She uses a feeding tube and requires 24-hour care.
Laparoscopic surgery is a safe and effective option for many patients, provided the surgeon knows the relevant anatomic landmarks and variations...
It is higher after elective primary cesarean.
How to prevent recurrent urinary tract infection in sexually active premenopausal women, postmenopausal patients, and women undergoing pelvic...
