Expert Commentary

Does vaginal prolapse repair using synthetic mesh confer long-term benefit over native-tissue colpopexy?
Not at this time.

SGS President Dr. Holly Richter had the great honor to present the best poster and video awards, as well as recognize the largest new-member class in the history of SGS. Dr. Norton was recognized for the best member presentation, which was on long-term prolapse follow-up in the TOMUS trial cohort. The FPRN was also recognized for their work on the impact of robotic hysterectomy in training.
The evening wrapped up with a lively social event in the exhibit hall with the meeting sponsors, colleagues, and friends.
3/24/14. Day 1 at SGS
Postgraduate course examines cautions and takeaways from published research
Our first day at the annual Society of Gynecologic Surgeons Scientific Meeting was off to a running start at the Postgraduate Courses. Program Chair Dr. Cheryl Iglesia joined me for a rapid-fire account of the evidence-based medicine course on social media.
The SGS birth on Twitter was explosive, with our four social media Fellow Scholars linking real-time comments to the courses. Dr. Vivian Sung put together an amazing team to review and apply the principles of evidence-based medicine for the course attendees. Once we accepted that most published research was bad and not terribly generalizable, small break-out groups were quick to use the PICO-S model to define (or try to define) a Population, Intervention, Comparator, Outcomes, and Study design.
This was followed by Dr. Ethan Balk of Tufts Center for Clinical Evidence Synthesis helping us wrap our heads around the randomized controlled trial (RCT). His caution was to consider the costly and underpowered trial, and lack of generalizability needed to define rigorous study inclusion and outcome criteria.
More bad news followed when Dr. Sung reviewed the cautionary tale of surrogate outcomes. While the perfect surrogate would allow us to shorten studies and save money, the seduction of association and causation can lead to some questionable conclusions. Are anatomical and urodynamic outcomes the same as patient perception of cure and improvement?
It wasn't all doom and gloom, as reflected in the lively tweets and posts by @obgmanagement and @gynsurgery. The strong work of the SGS Systemic Review Committee was lauded by Dr. Miles Murphy in his "How to Use a Clinical Practice Guideline." A systematic review needs to be included, though a meta-analysis is not always required, he said. What limits us is the poor quality and paucity of randomized trials for most patient populations. Treatment effect is best shown in RCTs, but minimizes harm; cohort and case series are better. Patient registries may allow for better determining a denominator and harm "rates," though they will miss clinical patient-based outcomes. With the coming of comparative effectiveness, these registries will be online quickly. Further, Dr. Balk showed us that, with more than 13,000 gynecologic research papers published each year, no one could ever keep track.
Dr. Ike Rahn gave an excellent presentation of subgroup analysis. To summarize: do it cautiously, describe which groups you analyze and have statistical back-up for your power and P-value calculations.
To round out the course, Dr. John Wong took us through his crystal ball on the future of evidence-based medicine. Because RCTs are expensive and comprise less than 2.5% of published studies, he proposed the analysis of observational studies as RCTs. Using patient-centered outcomes, efficacy data, and multiple providers, we will be better able to inform our patient and our colleagues on the best treatments. Again, as comparative effectiveness broadens policy decision, we must be agile, adaptive, and accountable.
Follow us on Twitter @obgmanagement #SGS14

Not at this time.
Laparoscopic surgery is a safe and effective option for many patients, provided the surgeon knows the relevant anatomic landmarks and variations...
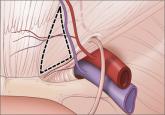
The most promising alternative to open power morcellation is morcellation in a bag, described here

Attention to the costs of the surgical devices, instruments, and related products you use can help ensure greater value for the care you provide—...
