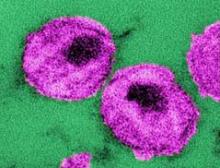
Allogeneic hematopoietic stem cell transplantation from HIV-naive individuals to HIV-1–positive individuals may achieve temporary antiretroviral-free remission of infection and loss of detectable HIV-1, a study showed.
Two men with chronic HIV-1 infection received allogeneic hematopoietic stem cell transplants (HSCTs) from susceptible donors to treat Hodgkin’s and non-Hodgkin’s lymphoma, and achieved temporary remission of HIV despite stopping antiretroviral therapy (ART), with the virus undetectable in both blood and rectal mucosa.
However, both experienced viral rebound – one at 12 weeks after stopping ART and one at 32 weeks – with both developing the usual symptoms of acute retroviral syndrome, according to a paper published online July 22 in the Annals of Internal Medicine.
"In summary, our results suggest that allogeneic HSCT with CCR5 wild-type donor cells may lead to loss of detectable HIV-1 from blood and rectal mucosa, but viral rebound may nevertheless occur after ART interruption despite a significant reduction in reservoir size," wrote Dr. Timothy J. Henrich of Brigham and Women’s Hospital, Boston, and his colleagues.
The researchers had previously reported the reduction in peripheral blood HIV-1 reservoirs in these two patients (Ann. Intern. Med. 2014 July 22 [doi:10.7326/M14-1027]).
"However, extensive sampling of tissues and large numbers of peripheral blood mononuclear cells for the presence of HIV-1 is necessary to understand the full effect of allogeneic HSCT on HIV-1 persistence," they wrote, arguing that treatment interruption was also necessary to establish if the virus was in remission.
Antiretroviral-free remission had previously been achieved in a patient who received an HSCT from a donor with a homozygous 32–base pair deletion in the gene encoding CCR5, a coreceptor for HIV-1. In this patient – known as "the Berlin patient" – remission has been maintained for more than 7 years, representing the only known functional cure of HIV infection.
The authors of the study suggested that while allogeneic HSCT may lead to significant and sustained reductions in the HIV-1 reservoir, the virus appears to persist in infected tissue or bound into cells, and those small numbers of infected cells were enough to restart HIV-1 replication.
Although both patients did experience rebound infection, that occurred much slower than it would have under normal circumstances, the authors said.
"Despite frequent sampling, neither of our patients had detectable HIV-1 in [peripheral blood mononuclear cells] or plasma for several months after ART discontinuation before viral rebound," they wrote.
Both patients received treatment for graft versus host disease after the transplant.
The study was supported by the Foundation for AIDS Research and the National Institute of Allergy and Infectious Diseases. Dr. Henrich had no disclosures. Some of the study’s other authors, as well as the editorial author, Dr. Lewin, declared grant support, speakers fees, and consulting fees from agencies and pharmaceutical companies.