Psychiatrists in the trenches are not alone in being unsure how to treat breakthrough bipolar depression. No panelist or other expert attending a recent American College of Neuropsychopharmacology symposium could definitively recommend:
- when to add an antidepressant to mood-stabilizer therapy
- whether to discontinue antidepressants after bipolar depression is stabilized.
Until controlled trials address these issues, we must use limited evidence to treat patients with bipolar depression. To help you meet this challenge, this article offers provisional suggestions based on recent published and unpublished reports.
Evidence for continuing
No published, randomized studies have examined how long to continue antidepressants after bipolar depression has stabilized. Until recently, conventional wisdom has been to discontinue antidepressants as soon as possible because of worries about antidepressant-induced mania. Then two case-controlled studies—one retrospective and one prospective—challenged that assumption.
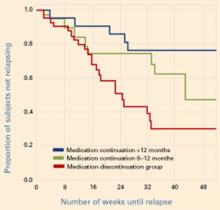
Figure Reduced relapse rates in patients whose antidepressants were continued
In a prospective case-controlled study, patients with bipolar disorder who continued antidepressant treatment for 6 to 12 months or >12 months after depressive episode remission had lower relapse rates than those who discontinued antidepressants within 6 months.
Source: Reprinted with permission from reference 2. Copyright 2003. American Psychiatric AssociationUsing similar methodologies, Altshuler et al1,2 examined bipolar patients who remained in remission for 6 weeks on mood stabilizers plus adjunctive antidepressants. Those who continued the antidepressants were less likely to relapse into depression (without an increase in manic episodes) than those whose antidepressants were discontinued (Figure).
Relapse rates in the first study1 were 35% at 1 year in those who continued antidepressants and 68% in those who did not. In the second study,2 36% and 70% of patients, respectively, had relapsed at 1 year. In the latter study, those who continued to take antidepressants for at least 6 months—instead of at least 12 months—had intermediate depressive relapse rates (53% for 6 months vs. 24% for 12 months).
When interpreting these data, keep several caveats in mind. For one, patients were not randomly assigned to continue or discontinue antidepressants but were designated by patient and clinician choice. When comparing the two patient groups, however, the authors found no inherent differences in illness characteristics that might have biased the results.
More importantly, few patients initially treated with antidepressant augmentation responded well and remained in remission. In the prospective study, 549 of 1,078 patients in the Stanley Foundation Bipolar Network received an antidepressant for breakthrough depressive symptoms.2 Only 189 remained on antidepressants for 2 months, and only 84 (15%) of the original population remained in remission for 2 months.
Summary. A small subgroup of patients appears to respond well to antidepressants and sustains this response for 6 to 8 weeks. For this subset, continuing antidepressant therapy would appear to be an appropriate strategy, based on:
- a significantly reduced risk for depressive relapse
- no increased risk of switching to mania, which is the usual reason to terminate antidepressants early.
Subsequent evidence
One needs to assess these observations in light of an interim analysis reported halfway through a small, open, randomized study. Ghaemi et al3 found no significant difference in outcomes—regardless of rapid-cycling status—among 14 bipolar patients who remained on antidepressants and 19 who discontinued across an average 60 and 50 weeks, respectively.
Table
Evidence on continuing antidepressants in breakthrough bipolar depression
| Study | Design | Results |
|---|---|---|
| Altshuler et al 1 | Retrospective, case-control, 39 patients (1 year) | Relapse rates: 35% in patients who continued antidepressants after mood stabilization and and 68% in those who did not; study included no rapid-cyclers |
| Altshuler et al 2 | Prospective, case control 84 patients (1 year) | Relapse rates: 36% in patients who continued antidepressants after mood stabilization and 70% in those who did not; study included no rapid cyclers |
| Ghaemi et al 3 (unpublished) | Open, randomized 33 patients (approx. 1 yr) | Relapse rate: 50% within 20 weeks, whether or not patients continued antidepressants; one-third of patients were rapid cyclers |
A survival analysis initially suggested some benefit for continuing antidepressants, but this disappeared when the authors adjusted for potential confounding factors—which was not done in the Altshuler et al studies. Patients receiving short-term or long-term antidepressants had a similar number of depressive episodes per year (1.00 vs. 0.75 episodes/year, respectively). For some reason, nonrapid-cycling patients showed greater depressive morbidity than those with rapid cycling.
Rapid cyclers comprised 30% of patients who continued antidepressants and 37% of those who discontinued. This may explain the 50% relapse rate within 20 weeks in both groups. By comparison, the Altshuler et al studies included no rapid cyclers.1,2 More details on this unpublished data are expected.
Are antidepressants the answer?