Interestingly, TD triggered by taking one atypical may respond to treatment with another. Suzuki et al15 reported that three patients who had developed early-onset TD while taking risperidone showed TD remission after risperidone was replaced by olanzapine in one patient and by quetiapine in the other two.
The atypicals are well tolerated but not without side effects. Weight gain is the most common problem and one with potentially serious health consequences.16
Using conventional agents. Even though atypicals are available, the clinician may consider continuing therapy with conventional antipsychotics in patients with TD when:
- the patient’s mental status has been satisfactory while taking conventional agents
- TD has been mild and stable over an extended time
- the patient has no side effects other than TD.
The literature supports the clinical experience that mild TD rarely worsens with continued antipsychotic therapy. Studies of 5 years or more tend to show TD stability with continued conventional antipsychotic therapy.17 It is prudent to maintain stable chronic psychotic patients with mild TD on the lowest effective dosages of conventional antipsychotics and to monitor them regularly for changes in dyskinesia and psychiatric status.
MANAGING COMPLICATED TD
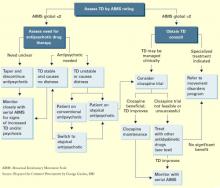
Managing severe TD or patients showing dystonia, tics, marked akathisia, or DIP coexisting with TD usually calls for more-aggressive interventions (Algorithm).
Algorithm Clinical management of tardive dyskinesia (TD)
Clozapine remains the first-line treatment for difficult TD; it has a very low propensity for inducing DIP and very rarely causes TD.18 Controlled studies,18,19 case reports, and open trials demonstrate its efficacy for reducing TD of all types and severity at a usual dosage of 300 to 500 mg/d. Clozapine’s antidyskinetic effects may be attributed to the absence of rebound after withdrawal and its greater efficacy in more-severe cases.18
Long-term clozapine therapy is recommended for TD, as symptoms remit slowly. Because weight gain, sedation, and other side effects—as well as mandatory blood monitoring—make clozapine less-than-ideal in clinical practice, researchers are seeking other effective therapies for TD.
Other atypicals. The obvious place to look is the other atypicals, which are simpler than clozapine to administer long-term. To date, however, these drugs have not proven to be as reliably effective as clozapine for TD. A recent review concluded that among the atypicals only clozapine induces less EPS than low-potency conventional antipsychotics.20
Nonantipsychotic agents. Other antidyskinetic drugs have come and gone; none has stood the test of time or proven effective in controlled trials. These agents may benefit some TD patients, but improvement is usually not dramatic.
Vitamin E was found to be effective in some TD treatment studies14 but not more effective than placebo in the largest controlled trial.21 Long-term treatment with dopamine-blocking antipsychotics is thought to cause oxidative stressinduced neurotoxicity in the nigrostriatal system.22 Lipid-soluble antioxidants such as vitamin E decrease free-radical formation, and it is possible that vitamin E may yet emerge as a helpful agent in preventing TD.23
Melatonin, a stronger antioxidant than vitamin E, was found to reduce TD in a 6-week placebocontrolled study,22 but the degree of TD improvement was modest. Melatonin’s value as a therapeutic agent for TD remains dubious.23
Miscellaneous. Case reports and studies with small series of TD patients have advanced numerous compounds as possible therapeutic agents (Table 2). Other drugs that occasionally have shown benefit in TD include buspirone, propranolol, pyridoxine (vitamin B6), ondansetron, clonidine, and the neuropeptide ceruletide.
ECT and diet. Suggested nondrug treatments of TD include electroconvulsive therapy (ECT)14 and a diet of mixed branched-chain amino acids.24
Table 2
Compounds that occasionally show benefit in TD
| Class | Example |
|---|---|
| Cholinergics | Lecithin |
| Catecholamine depletors | Tetrabenazine (investigational orphan drug) |
| Calcium channel blockers | Verapamil |
| Gabaergic compounds | Baclofen |
| Benzodiazepines | Clonazepam |
MANAGING TD VARIANTS
TD variants are notoriously difficult to treat but tend to respond to clozapine.18 In addition:
- Tardive dystonia is often treated with reserpine, tetrabenazine, or high doses of anticholinergic drugs.25 Botulinum toxin A injections into affected muscles may be remarkably effective but must be repeated regularly.25
- Tardive akathisia may improve slowly with clozapine, propranolol, or benzodiazepines.25
Managing severe or atypical TD is usually beyond the expertise of the practicing psychiatrist. Obtaining consultation from a psychopharmacologist or a neurologist experienced in treating movement disorders is highly recommended.
PREVENTING TD
Conventional antipsychotics are still prescribed by psychiatrists, internists, and family physicians and are often given in emergency rooms. Avoiding these drugs whenever possible and using the lowest effective dosages will reduce the risk of TD.26
Patients at relatively high risk for TD—the elderly, those who are very sensitive to acute EPS, and those with affective disorders or diabetes mellitus—are rarely candidates for conventional neuroleptics if a suitable alternative exists. Genetic research may further identify individuals susceptible to TD.27