Other promising psychotherapeutic interventions include supportive-expressed group therapy, in which a group of advanced cancer patients meets with a mental health professional and discusses goals of building bonds, refining life’s priorities, and “detoxifying” the experience of death and dying.19 A primary purpose of this therapy is not just to foster improved relationships within a group of cancer patients, but also within their family and oncology team, with the aim of improving compliance with anticancer therapies. Nurse-delivered, one-on-one sessions focusing on depression education, problem-solving, coping techniques, and telecare management of pain and depression also improves outcomes among depressed cancer patients.20
Hospital-based inpatient and outpatient palliative care consultation teams are becoming more common. A randomized controlled trial of early palliative care outpatient consultation for patients with incurable lung cancer showed improved depression outcomes, better quality of life, and a modest improvement in survival.21 Although the most effective elements of a palliative care consult remain unspecified and require further research, improvement in outcomes may result from more effective symptom management, better acknowledgement of the burden of illness on the patient or family, or reduced need for hospitalization. Therefore, mental health professionals should consider palliative care consultation for advanced cancer patients with signs of psychological distress.
Pharmacotherapy options
Antidepressants. Patients with excessive guilt, anhedonia, hopelessness, or ruminative thinking along with a related impairment in quality of life may benefit from pharmacotherapy regardless of whether they meet diagnostic criteria for MDD. Although SSRIs and SNRIs have become a mainstay in managing depression, placebo-controlled trials have yielded mixed results in depressed cancer patients. Furthermore, differences in efficacy among these antidepressants may not be significant, according to a recent meta-analysis.22
Select an antidepressant based on the patient’s past treatment response, target symptoms, and potential for adverse events. Mirtazapine has relatively few drug interactions; the side effects of sedation and weight gain may be welcome among patients with insomnia and impaired appetite.23 Furthermore, mirtazapine is a 5-HT3 receptor antagonist,24 which suggests it might act as an effective antiemetic.25 Other SNRIs, such as venlafaxine and duloxetine, have demonstrated benefits in managing neuropathic pain in patients who do not have cancer.26
Psychostimulants. Patients with a prognosis of days or weeks might not have enough time for an antidepressant to achieve full effect. Open prospective trials and pilot studies have shown that psychostimulants can improve cancer-related fatigue and quality of life while also augmenting the action of antidepressants.27 Psychostimulants, such as methylphenidate, have been used for treating cancer-related fatigue and depressive symptoms in medically ill patients. Their rapid onset of action, coupled with minimal side effect profile, make them a good choice for seriously ill patients with significant neurovegetative symptoms of a depressive disorder. Note: Avoid psychostimulants in patients with delirium and use with caution in patients with heart disease.28
Novel agents. A growing body of preclinical research suggests that glutamate may be involved in the pathophysiology of MDD. Ketamine modulates glutamate neurotransmission as an N-methyl-d-aspartate receptor antagonist. A recent evaluation of a single dose IV of ketamine in a placebo-controlled, double-blind trial found that depressed patients receiving ketamine experienced significant improvement their depressive symptoms.29 Irwin and Iglewicz30 describe 2 hospice patients administered a single oral dose of ketamine, which provided rapid relief of depressive symptoms and was well tolerated.
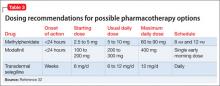
Transdermal selegiline may help patients who have trouble taking oral medications, including antidepressants. Inability to tolerate or absorb medications may be related to several conditions such as head and neck cancer, severe mucositis, and dysphagia. The dose-related dietary requirements—tyramine restriction—and careful monitoring for drug interactions may limit the use of selegiline in medically ill patients.31Table 3 features a list of dosing recommendations for pharmacotherapeutic options.32
Use the strategy of “start low, go slow” when initiating and adjusting antidepressants because patients with cancer and other advanced illnesses often have concomitant organ failure and are at risk of drug interactions. Carefully review your patient’s medication list for agents that are no longer beneficial or possibly contributing to depressive symptoms to help reduce the risk of adverse pharmacokinetic and pharmaco-dynamic interactions.
Requests for a hastened death
As many as 8.5% of terminally ill patients have a sustained and pervasive wish for an early death.33 Although requests for a hastened death may evoke strong emotional reactions and compel many clinicians to recoil or harshly reject such requests, consider such requests as an opportunity to gain insight into the patient’s narrative of his (her) suffering. The clinician’s role in such cases is to identify suicidality and perform a thorough suicide risk assessment. Interventions to prevent suicide should attempt to balance the seriousness of self-harm threats with restrictions on the patient’s liberty.34